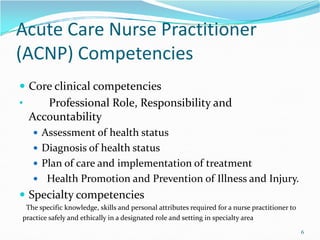
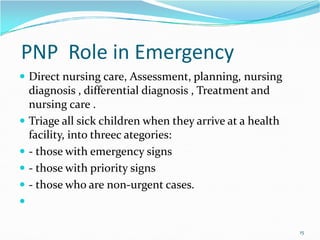
The document outlines the objectives and competencies required for advanced management of acute pediatric problems, emphasizing the nurse practitioner's role in assessment, diagnosis, and emergency management. Key areas include collaboration, communication, and the integration of evidence-based practices in healthcare. It also discusses the challenges faced by nurse practitioners in acute care settings and the importance of leadership and research in improving patient outcomes.