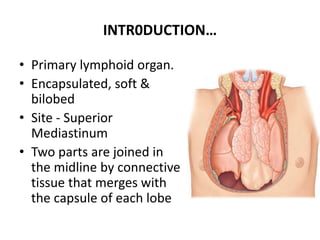
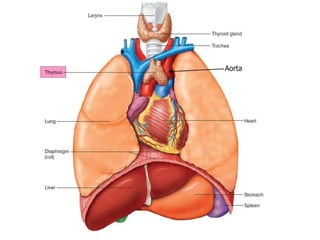
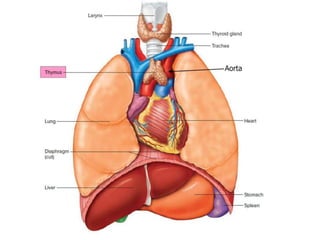
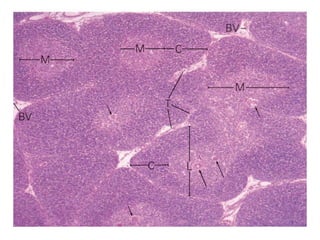
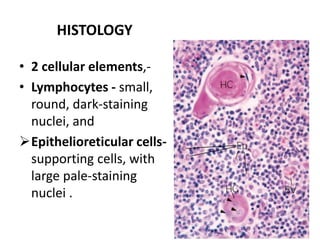
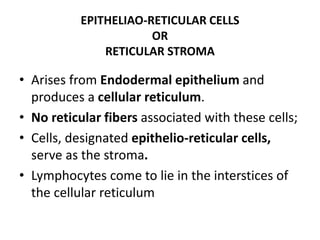
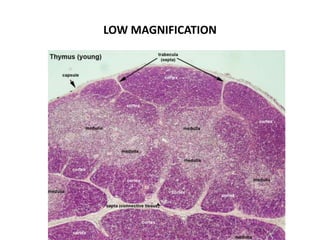
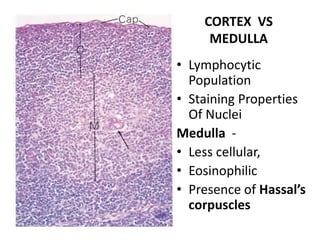
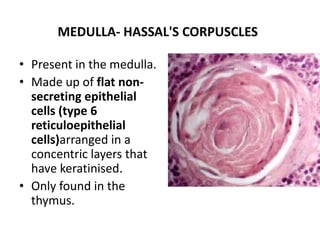
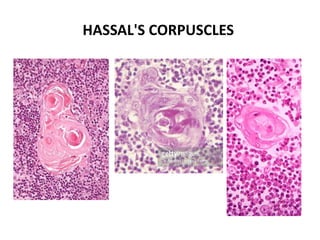
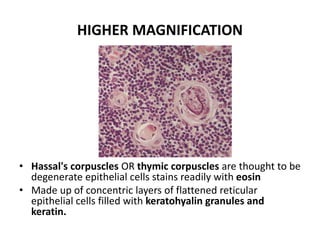
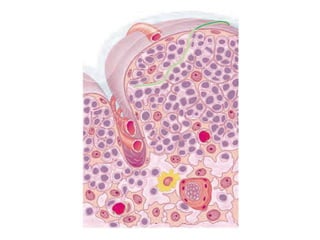
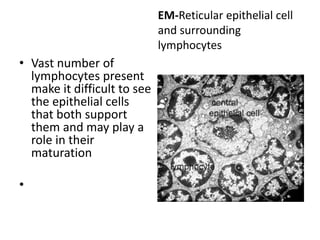
The thymus is a primary lymphoid organ located in the superior mediastinum. It plays a key role in T cell development and maturation. The thymus has an outer capsule and is divided into lobules containing cortex and medulla regions. The cortex contains densely packed developing T cells and epithelioreticular cells. The medulla is less cellular and contains Hassall's corpuscles. Developing lymphocytes interact with epithelioreticular cells, which provide structural support and signals to guide T cell maturation.