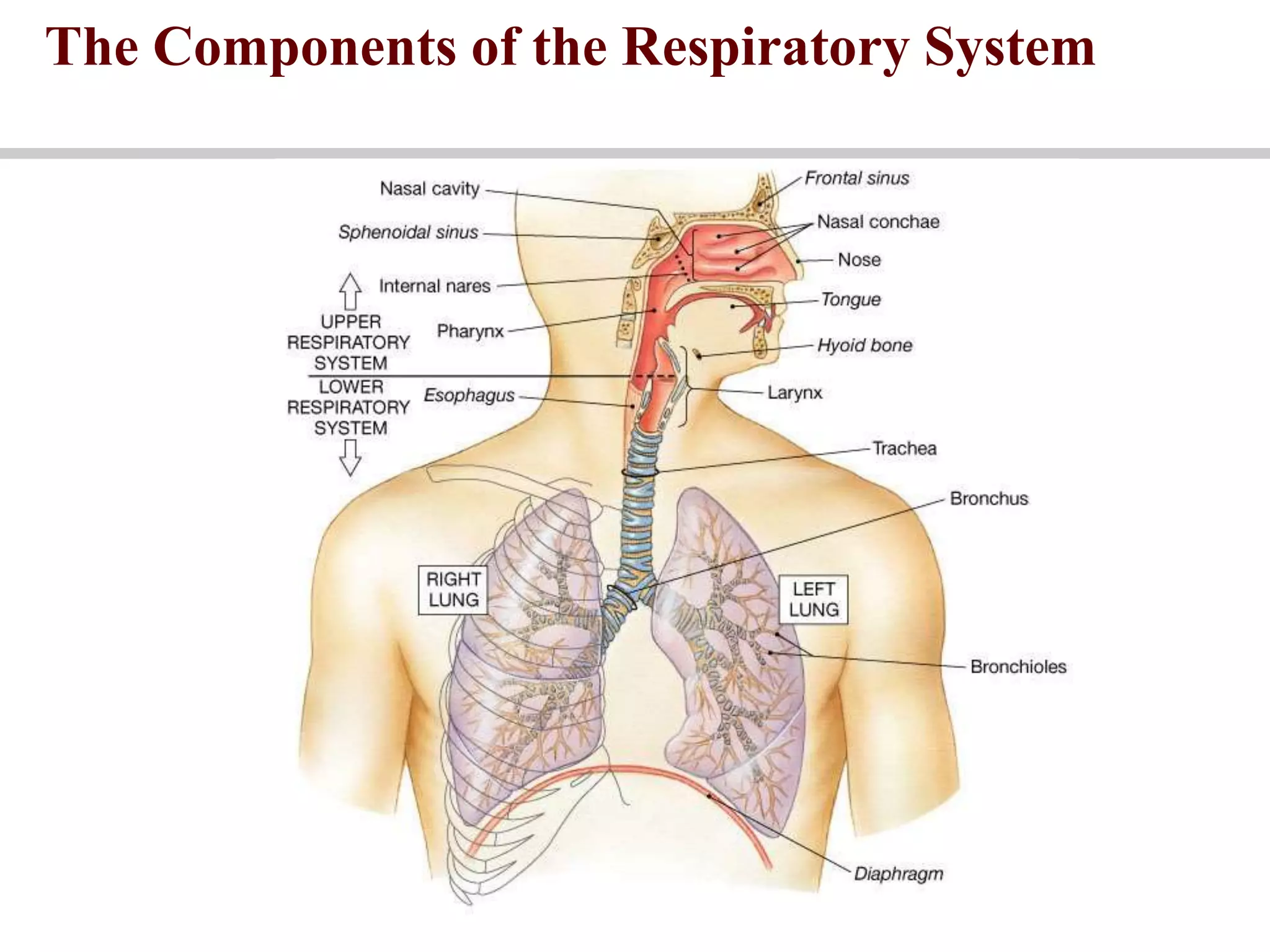
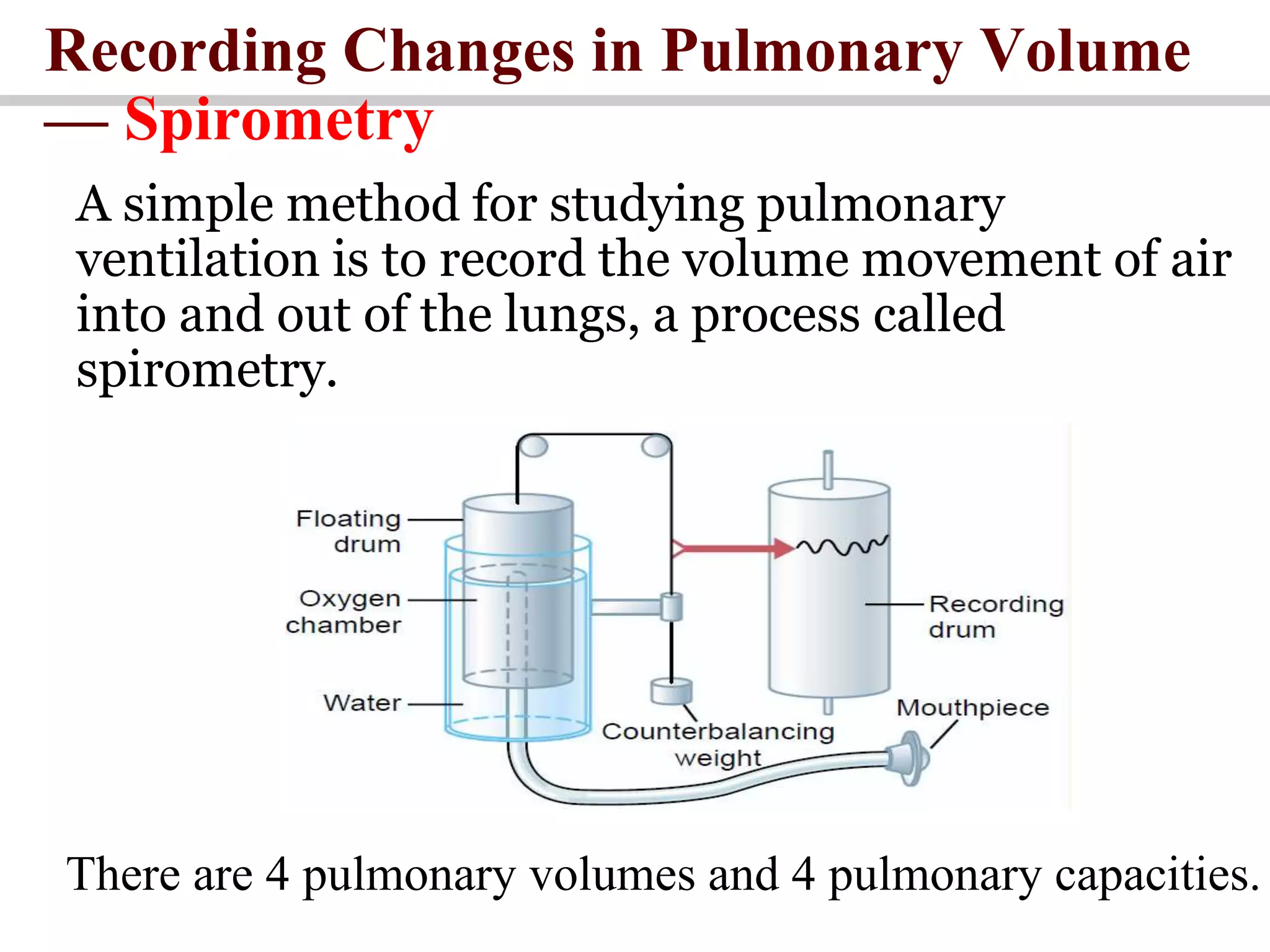
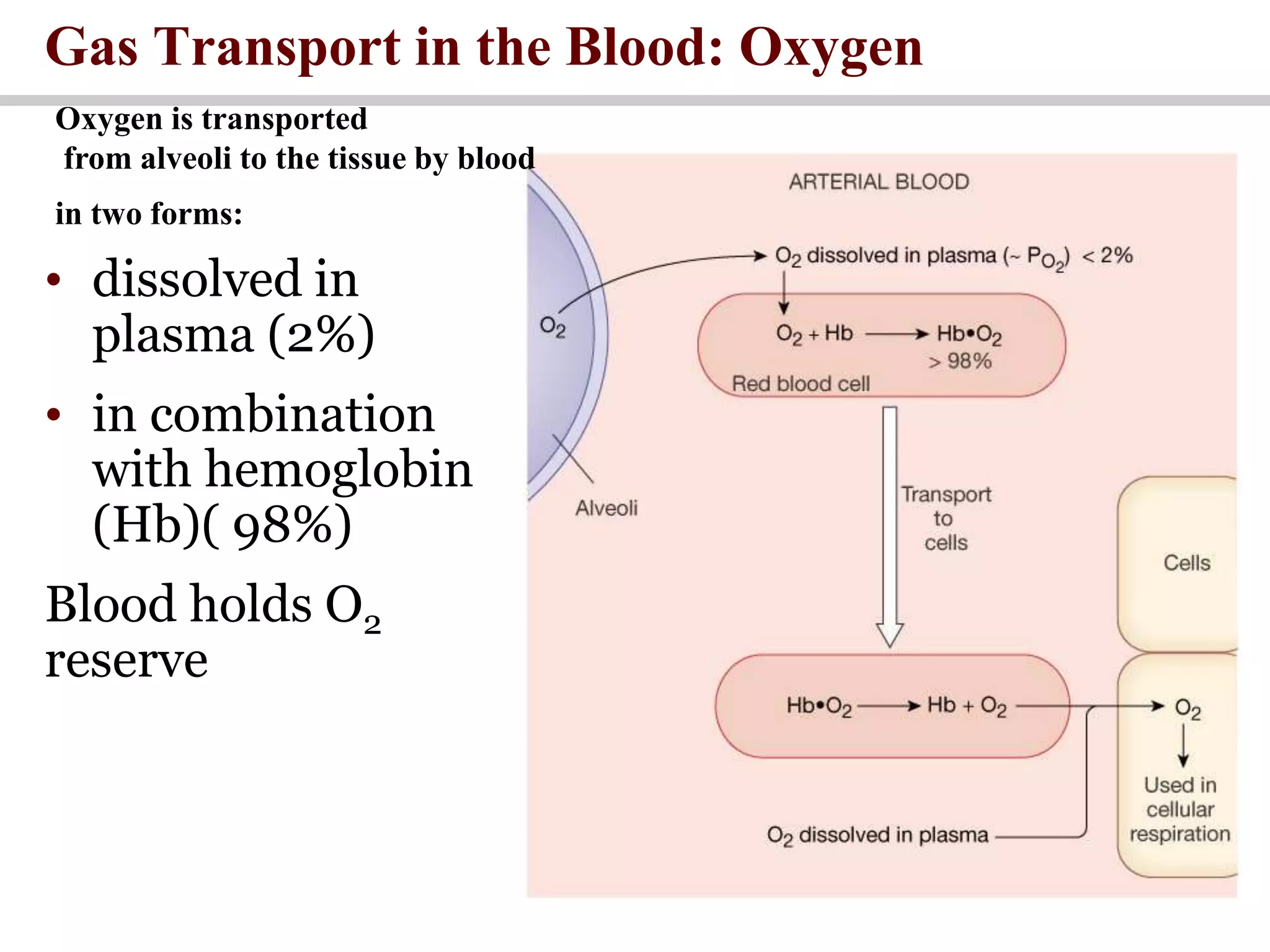
This document provides an overview of respiratory physiology, covering the definition and function of respiration, the steps of respiration, the structure and function of the conducting and respiratory zones of the lungs, lung volumes and capacities, mechanics of breathing, gas exchange, transport of oxygen and carbon dioxide in the blood and tissues, and control of breathing. Key points include that respiration involves the exchange of oxygen and carbon dioxide between the environment and body cells, occurring in five steps including ventilation, diffusion, transport, and cellular respiration. Gas exchange takes place in the alveoli via differences in partial pressures and is facilitated by a large surface area and thin diffusion barrier. Oxygen is transported in both dissolved and hemoglobin-bound forms in the blood, while carbon