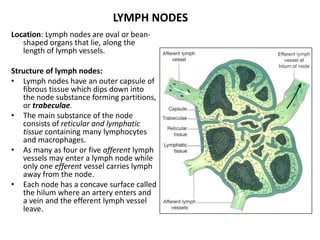
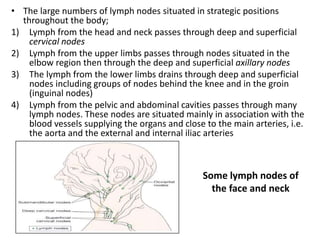
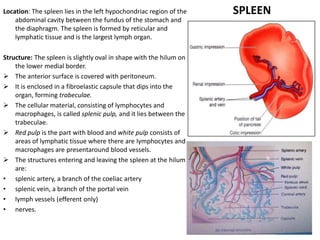
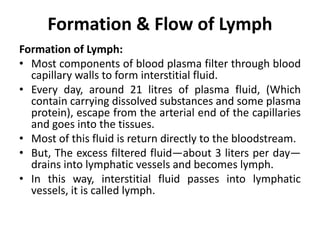
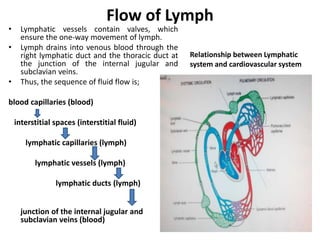
The lymphatic system consists of lymph, lymphatic vessels, lymph nodes, and lymphatic tissues. Lymph is formed from interstitial fluid that has filtered from blood capillaries. It is transported unidirectionally through lymphatic vessels by skeletal muscle and respiratory pumping action. Lymph vessels branch and join, eventually forming two main ducts that drain into veins in the neck. Lymph passes through lymph nodes, which filter lymph and activate immune cells. Together with organs like the spleen and thymus, the lymphatic system helps maintain fluid balance, absorb fats, and fight infection.