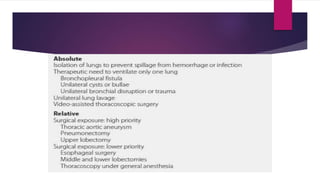
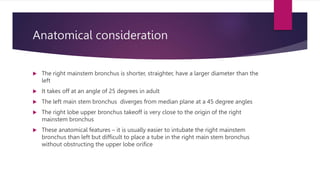
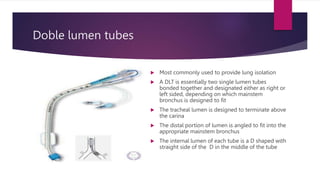
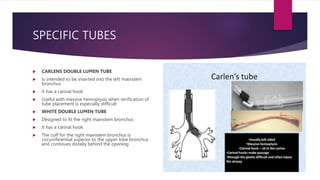
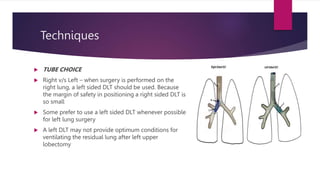
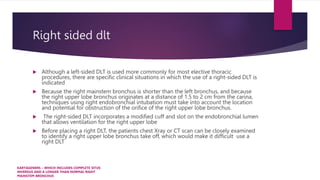
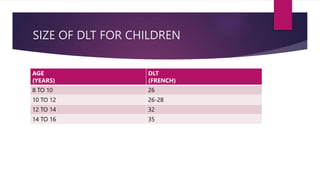
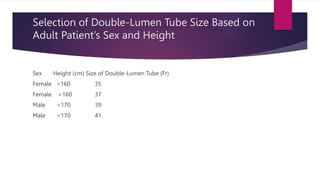
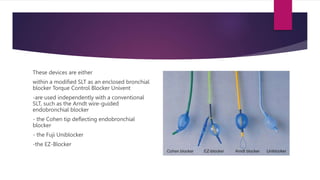
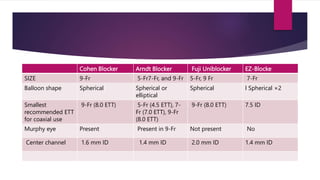
Lung isolation techniques are employed to facilitate one-lung ventilation (OLV) during various thoracic surgeries and to protect the lung from contamination or hemorrhage. The document details the anatomical considerations, types of double-lumen tubes (DLTs), indications for use, sizing recommendations, preparation, positioning, and potential complications associated with lung isolation methods. It also discusses the utility of bronchial blockers as an alternative for patients with complicated airways or previous lung surgeries.