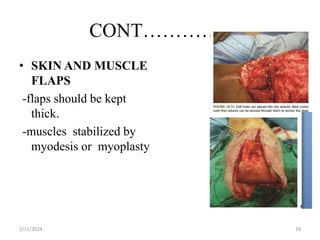
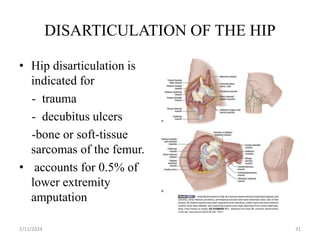
The document discusses principles of lower limb amputation. It covers the anatomy of the lower limb, indications and contraindications for amputation, pre-operative evaluation and preparation, surgical techniques for different types of amputations, post-operative care and complications, and the importance of rehabilitation. Key points include that over 185,000 amputations are performed in the US each year primarily due to peripheral artery disease, the goal of amputation is to remove non-viable tissue while preserving viable tissue for prosthetic fitting, and multidisciplinary rehabilitation is important for returning patients to functional status.