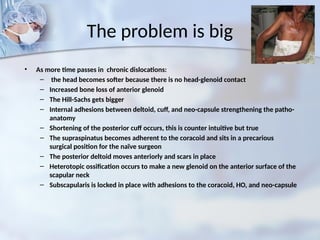
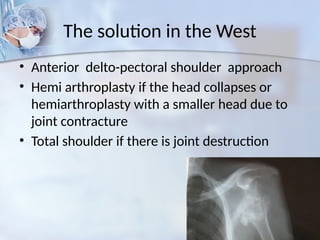
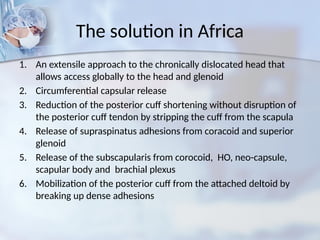
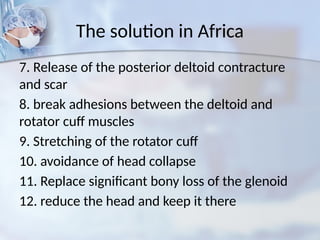
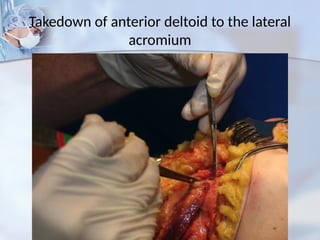
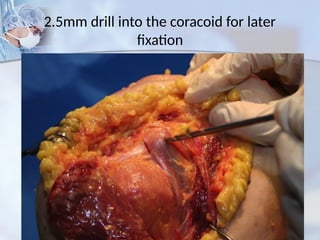
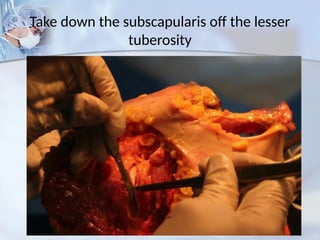
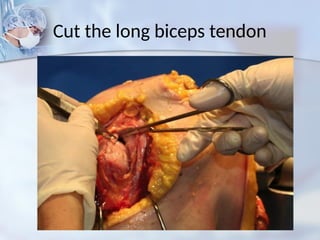
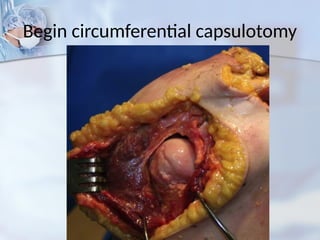
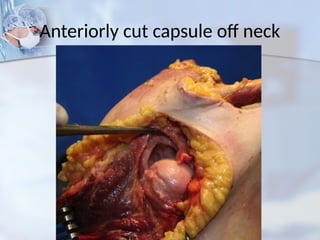
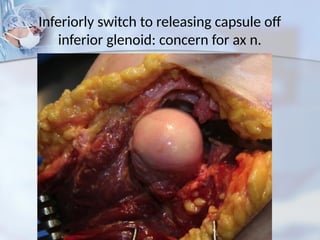
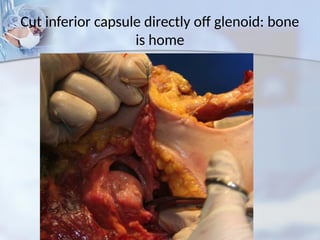
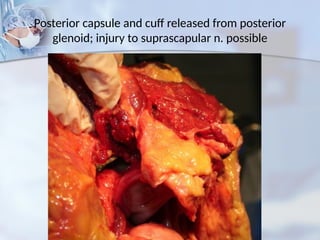
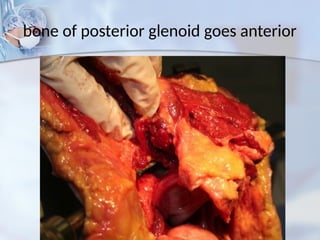
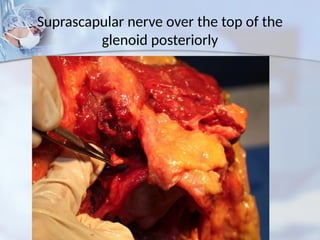
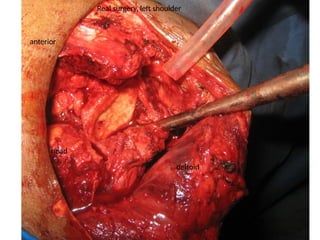
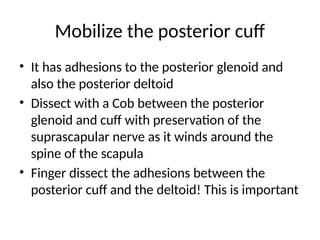
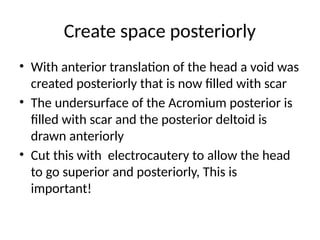
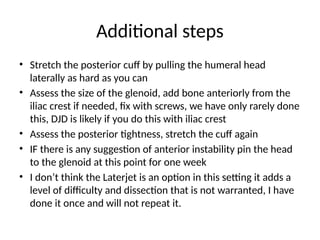
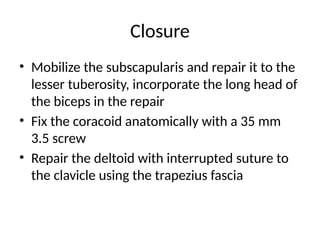
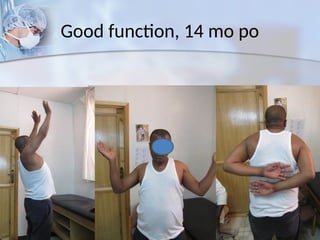
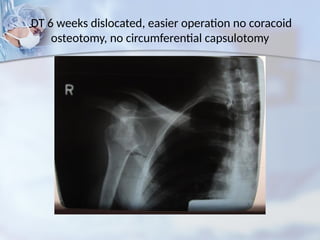
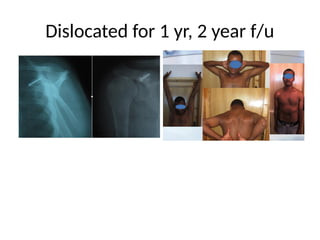
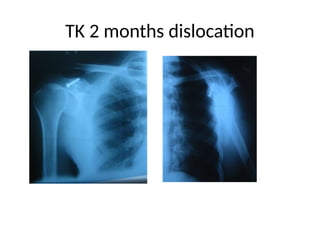
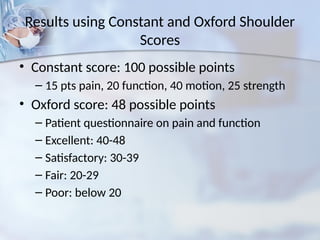
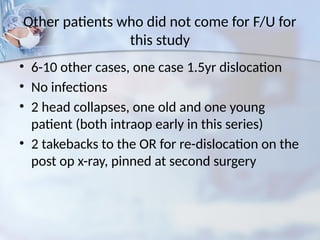
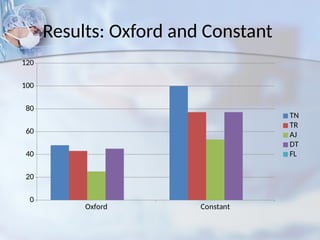
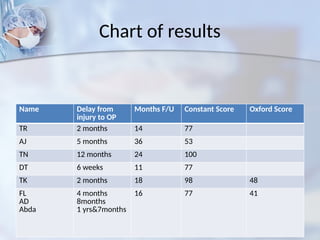
The document discusses a surgical technique for the open reduction of chronic shoulder dislocation, especially in under-resourced settings, highlighting the need for extensive capsular release and rotator cuff mobilization. It presents early results from various cases, showing that with adequate exposure and addressing multiple contractures, significant functional improvements can be achieved. The findings emphasize the complexity of the procedure and the importance of managing adhesions and bony loss in these patients.