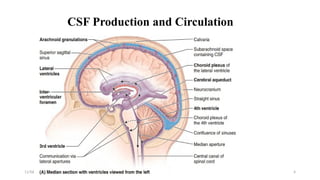
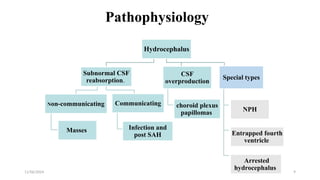
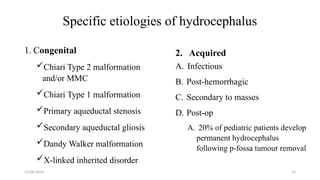
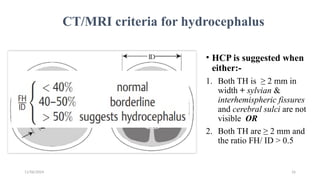
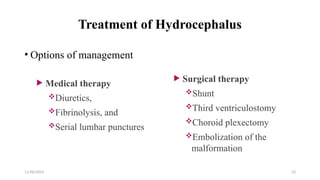
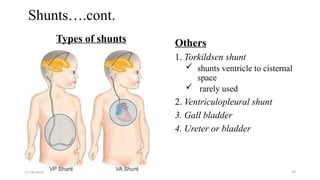
The document outlines hydrocephalus, its anatomy, physiology, causes, clinical features, diagnosis, and management strategies. Hydrocephalus, characterized by abnormal CSF accumulation in the brain, can lead to increased intracranial pressure and requires careful medical or surgical intervention. It emphasizes the importance of early treatment to prevent neurological impairment and the necessity for lifelong follow-up to monitor for complications.