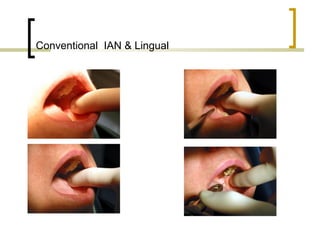
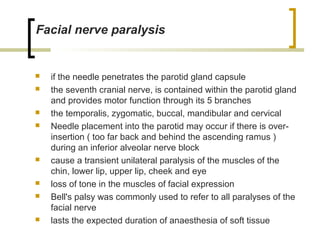
This document provides a historical overview of local anesthesia techniques from the 18th century introduction of chemical compounds to modern developments. It discusses key events and discoveries such as the first use of nitrous oxide and ether for dental procedures. The era of inhalation anesthesia gave way to injection techniques using hypodermic syringes and localized drugs like cocaine and procaine. Modern techniques for mandibular nerve blocks and vasoconstrictors that prolong anesthesia are also covered. The document concludes with sections on interactions, side effects, contraindications and toxicity of local anesthetic drugs and recommended maximum dosing.