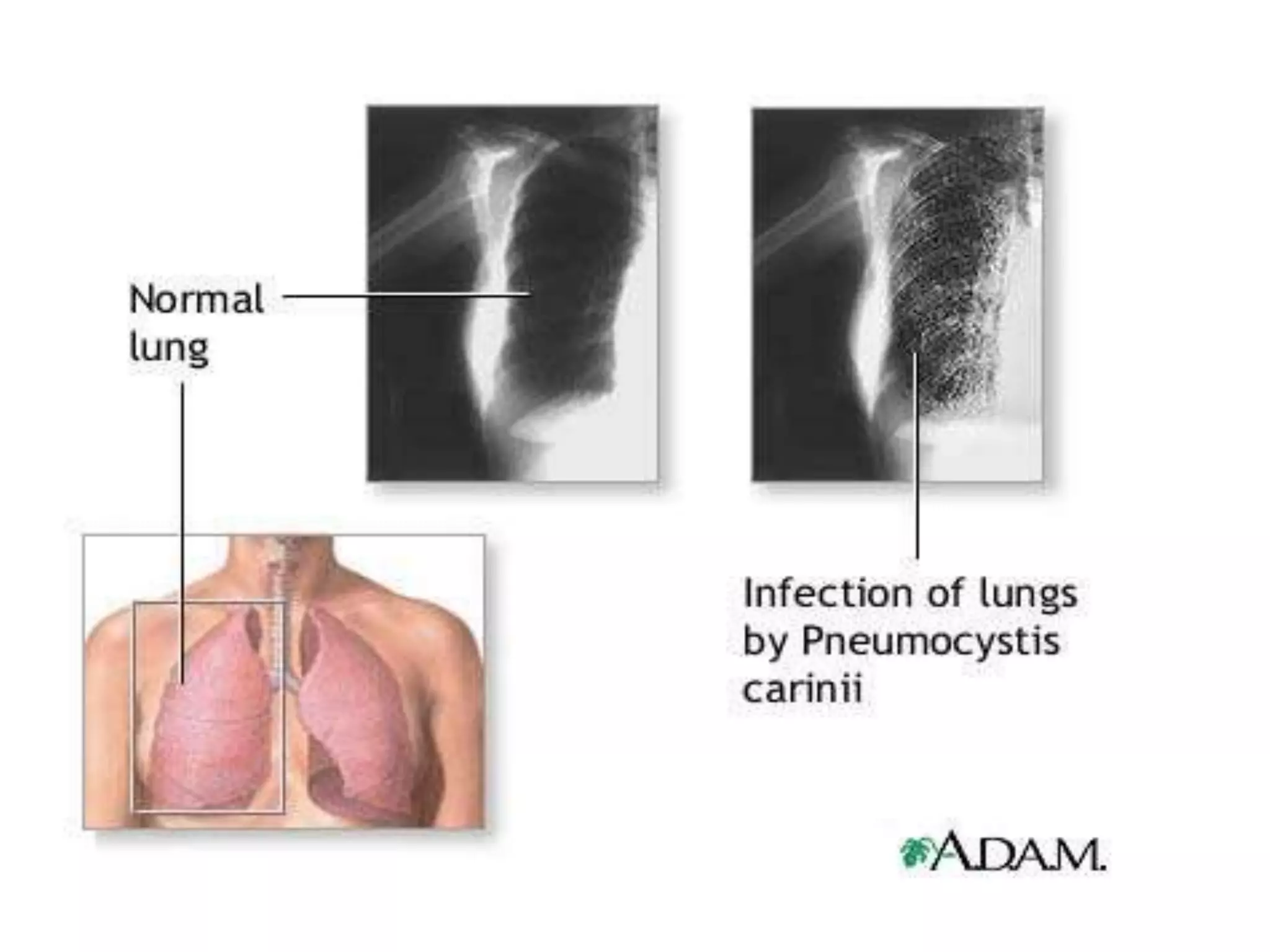
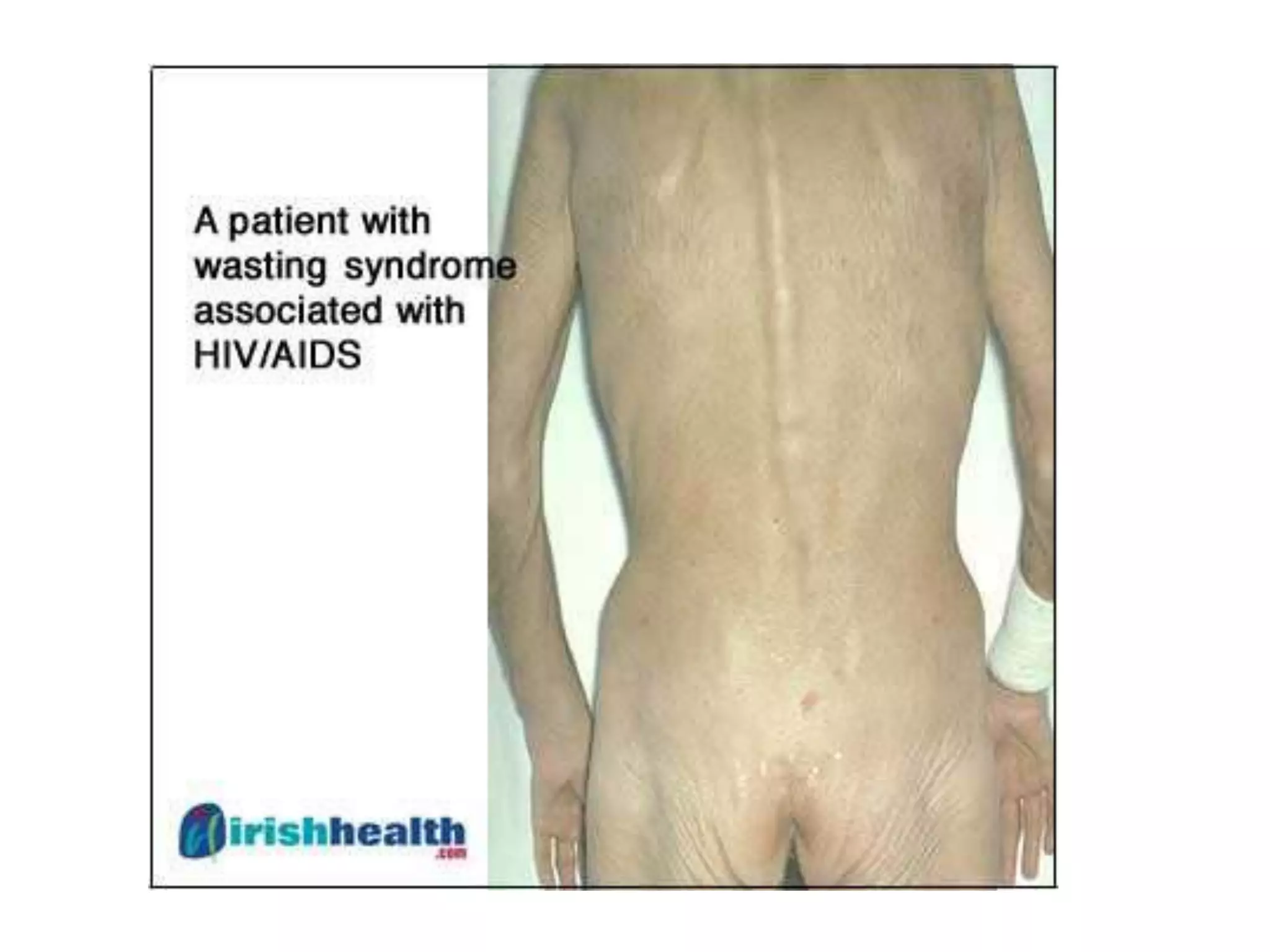
Pneumocystis carinii pneumonia is a common opportunistic lung infection caused by a fungus that takes advantage of weakened immune systems. Symptoms include nonproductive cough, fever, shortness of breath, and weight loss. Treatment involves trimethoprim-sulfamethoxazole and steroids. Mycobacterium avium complex is another opportunistic pathogen causing respiratory infections in immunocompromised individuals. Wasting syndrome is defined by over 10% involuntary weight loss and chronic diarrhea for more than 30 days. Kaposi's sarcoma is an HIV-related cancer affecting blood and lymph vessels. Cryptococcal meningitis presents with fever, headache, and neck stiffness. Highly active antiretro