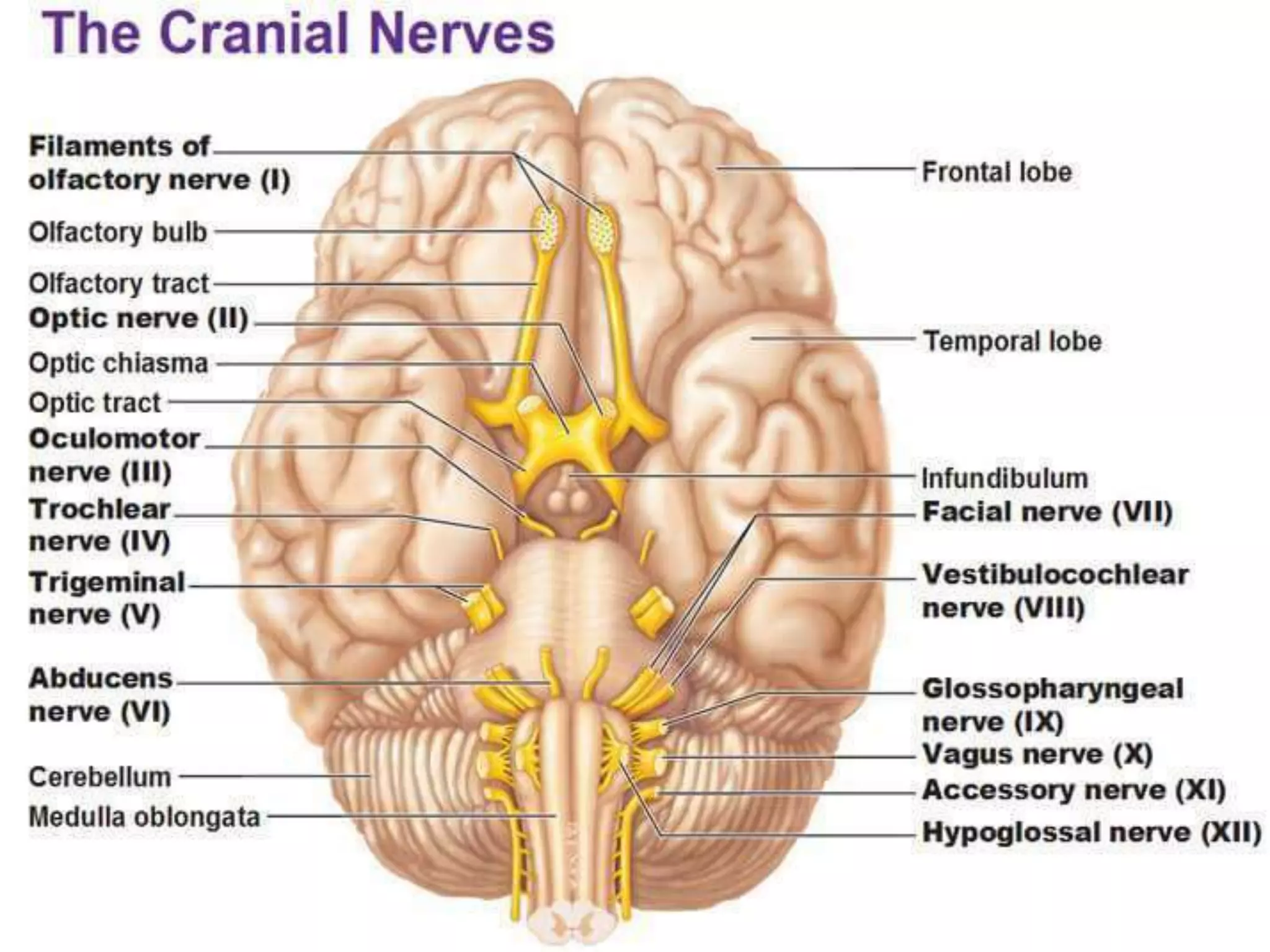
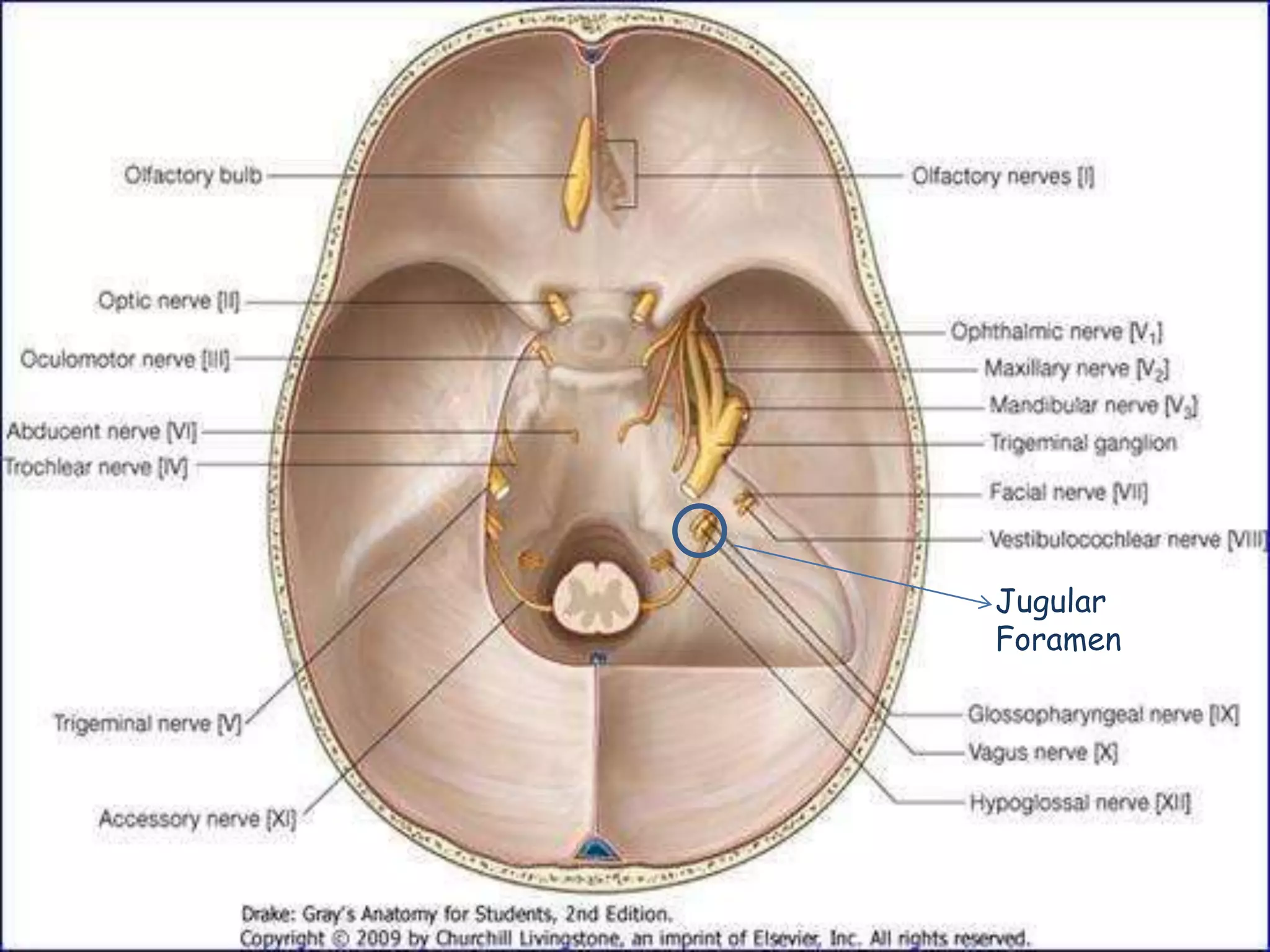
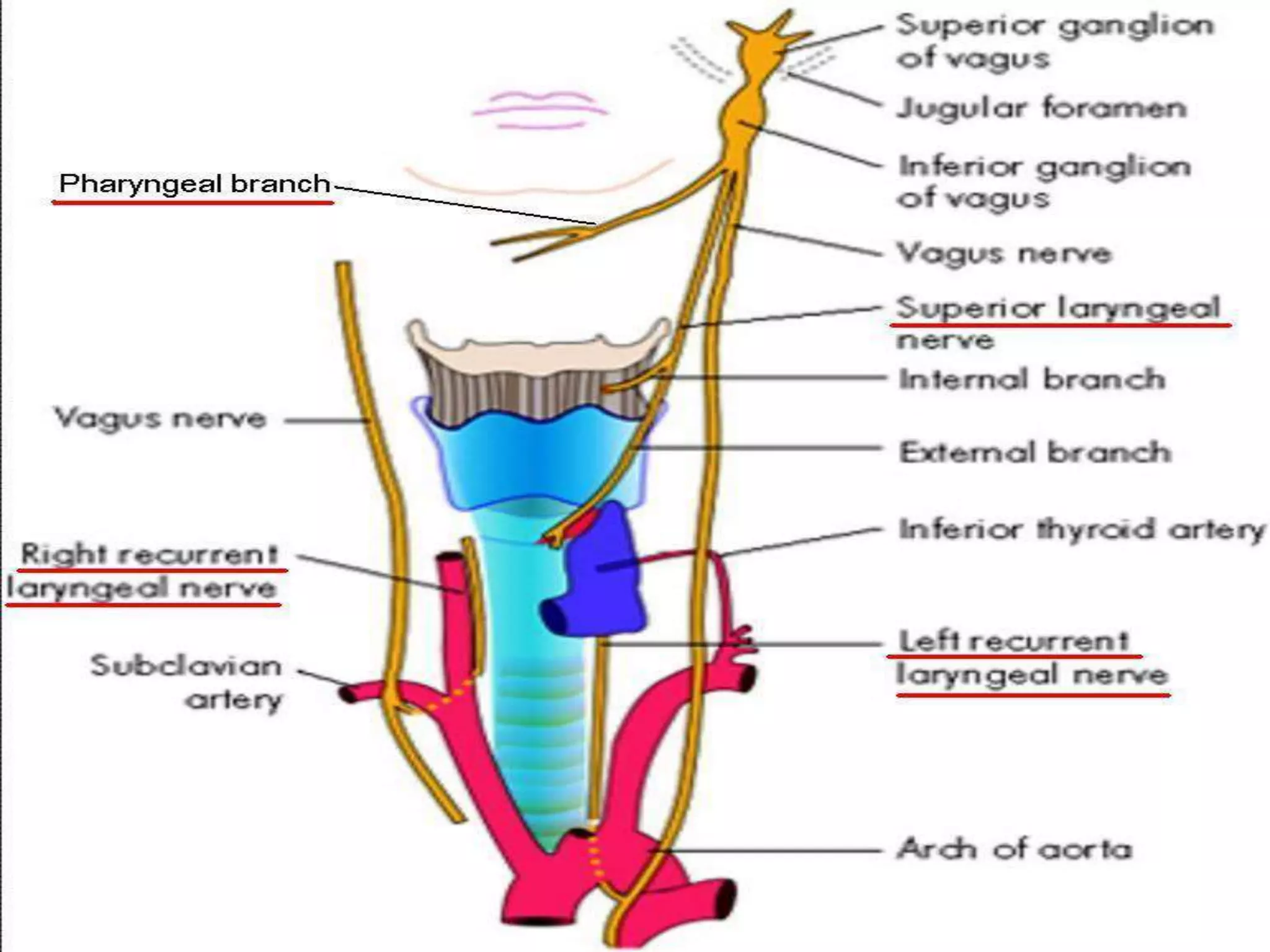
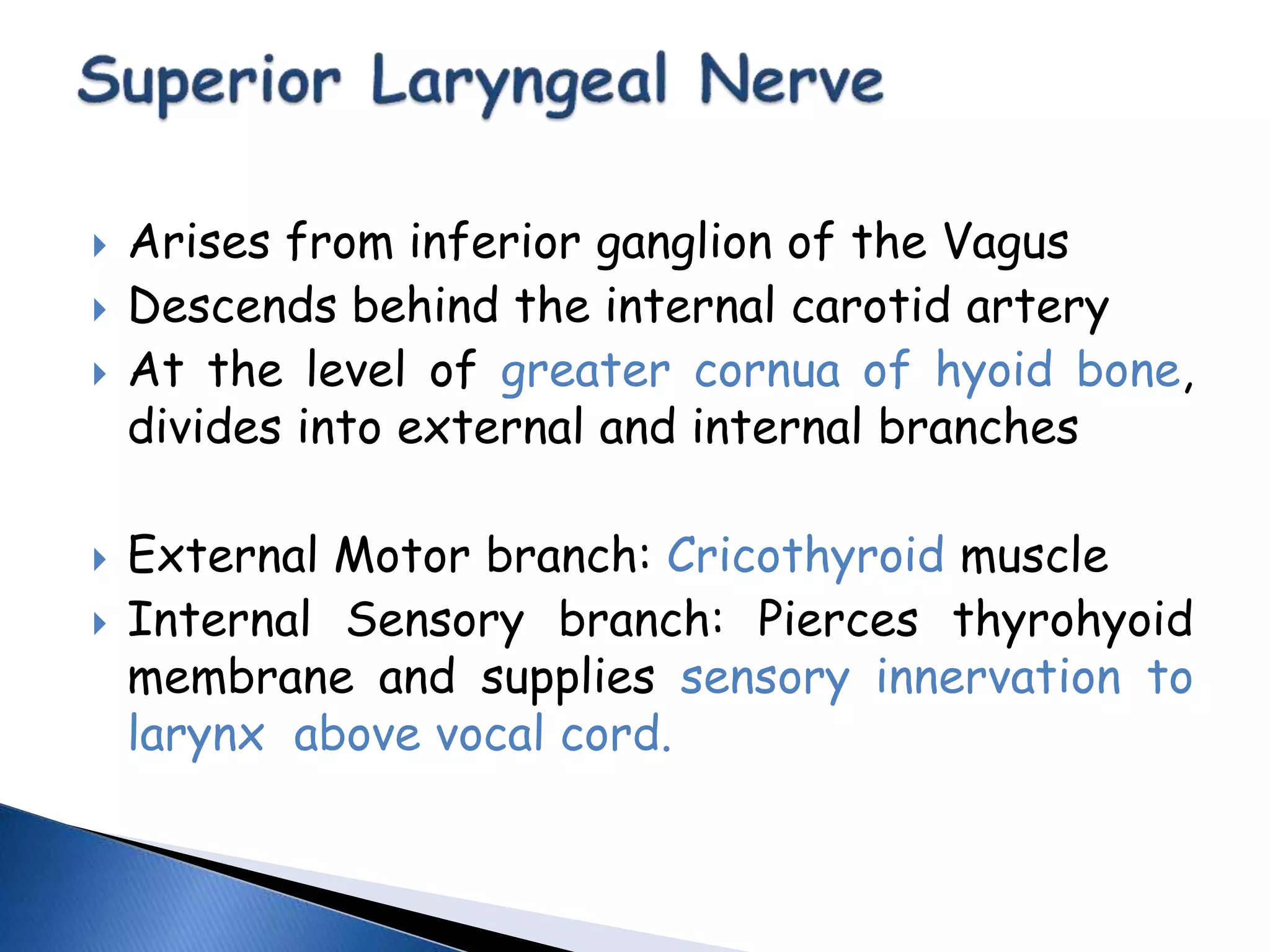
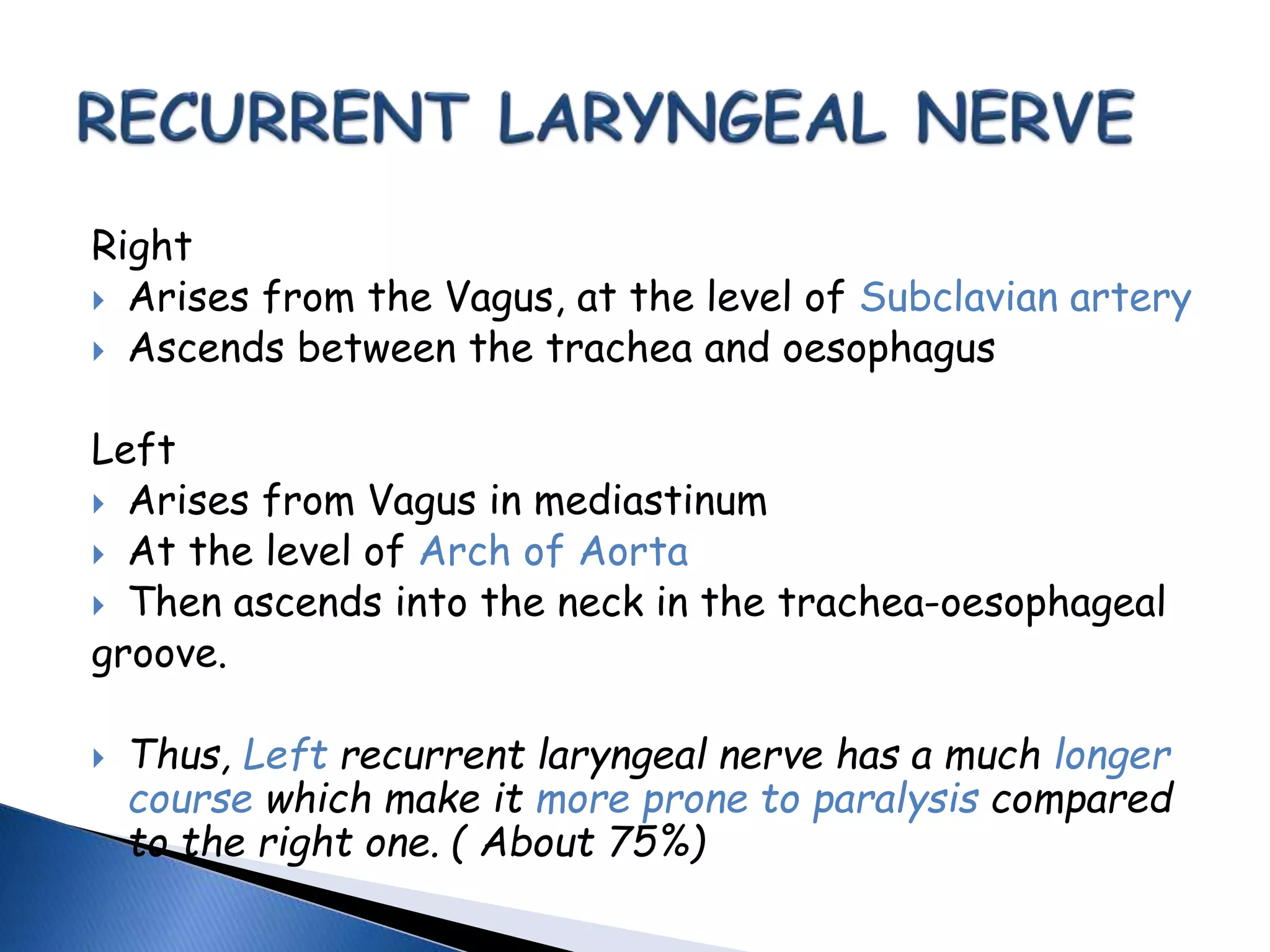
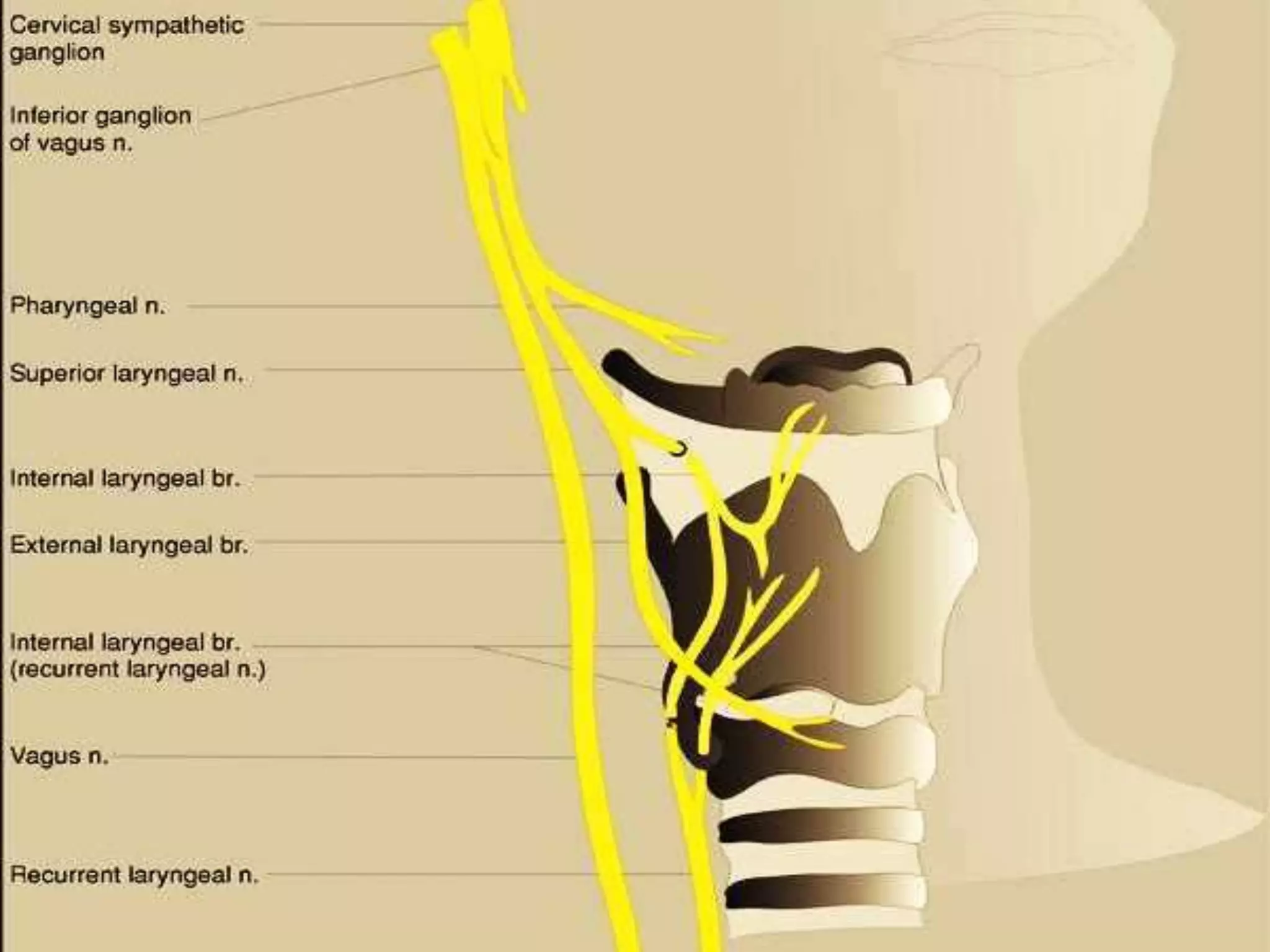
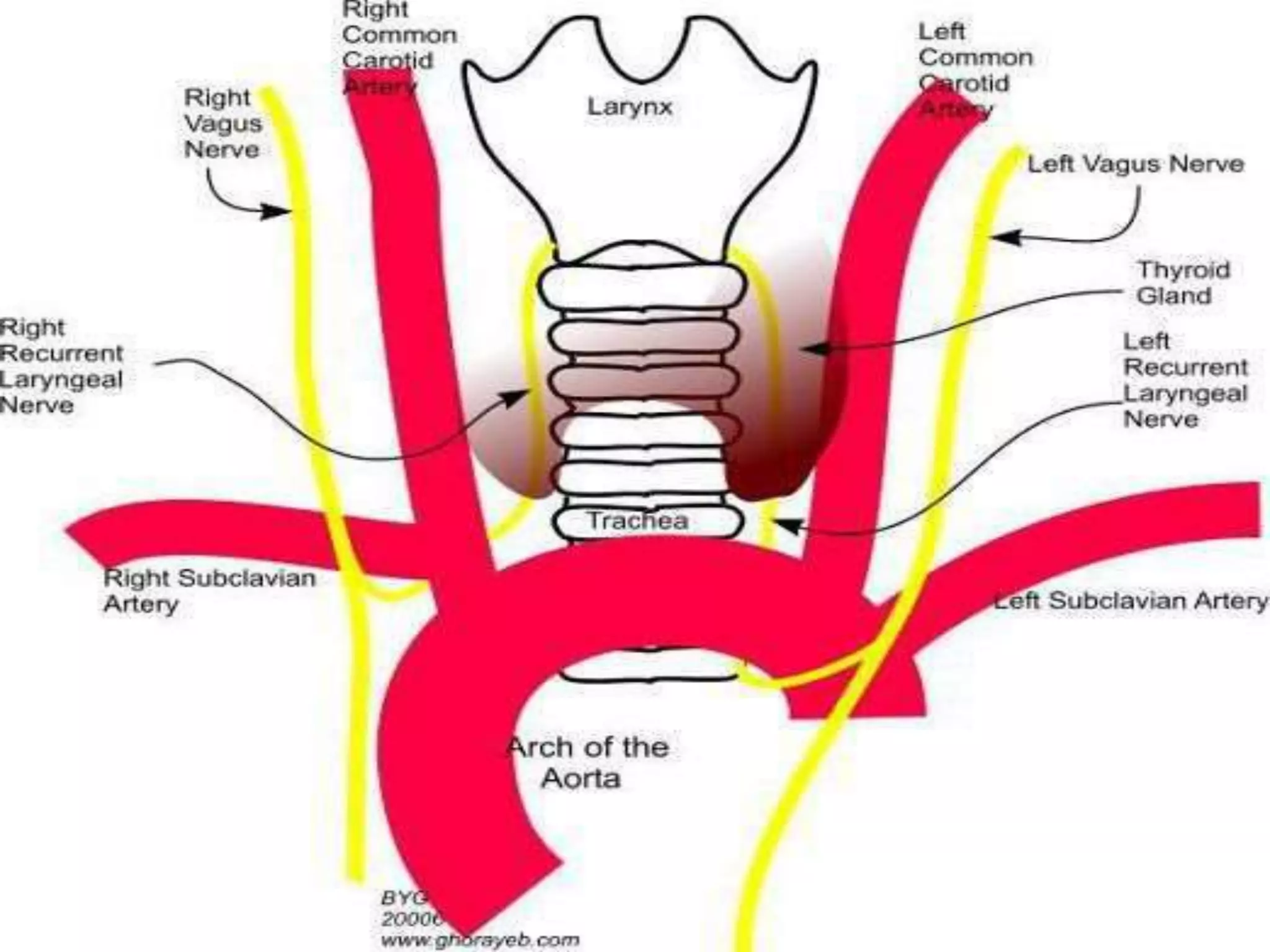
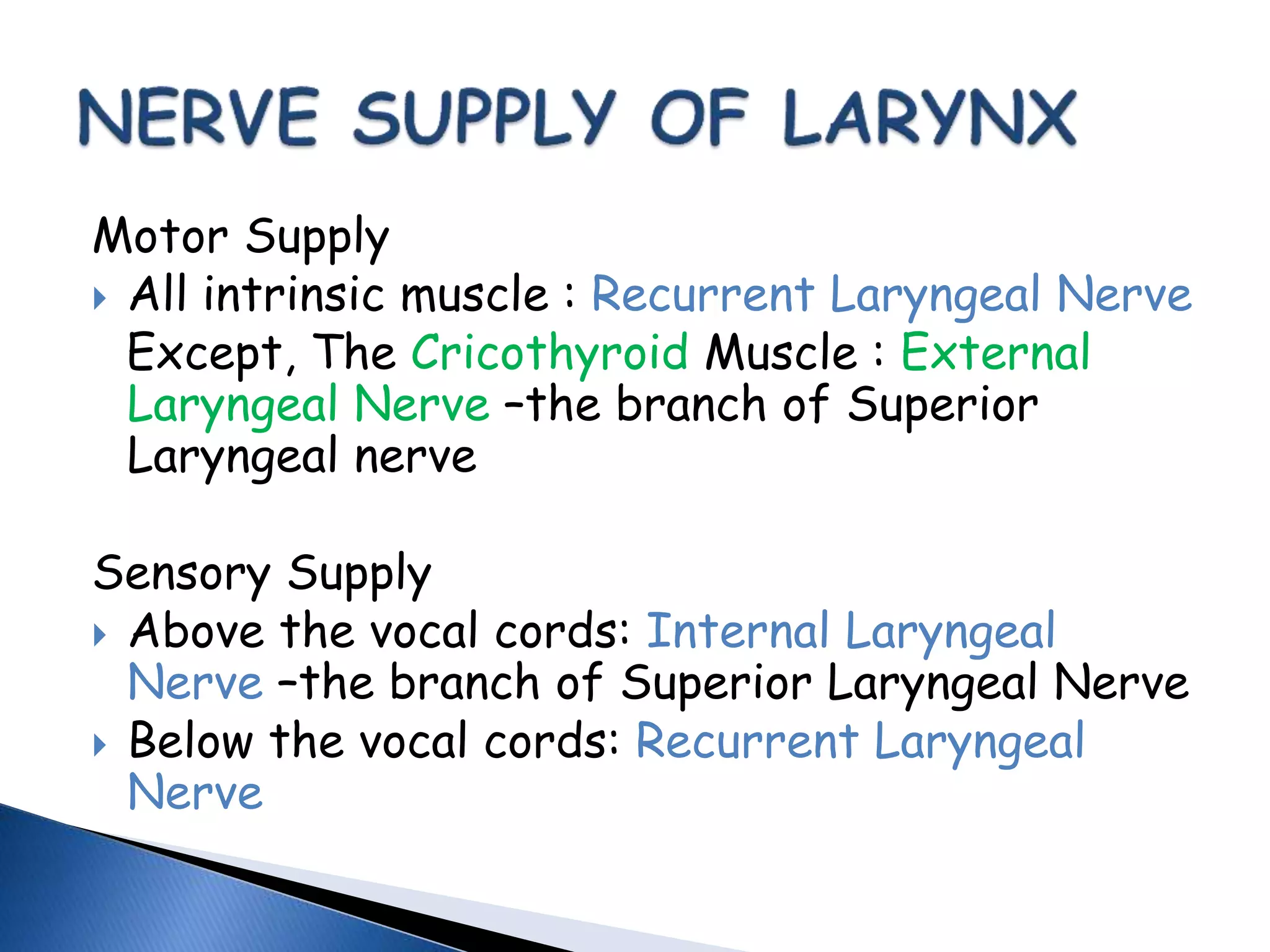
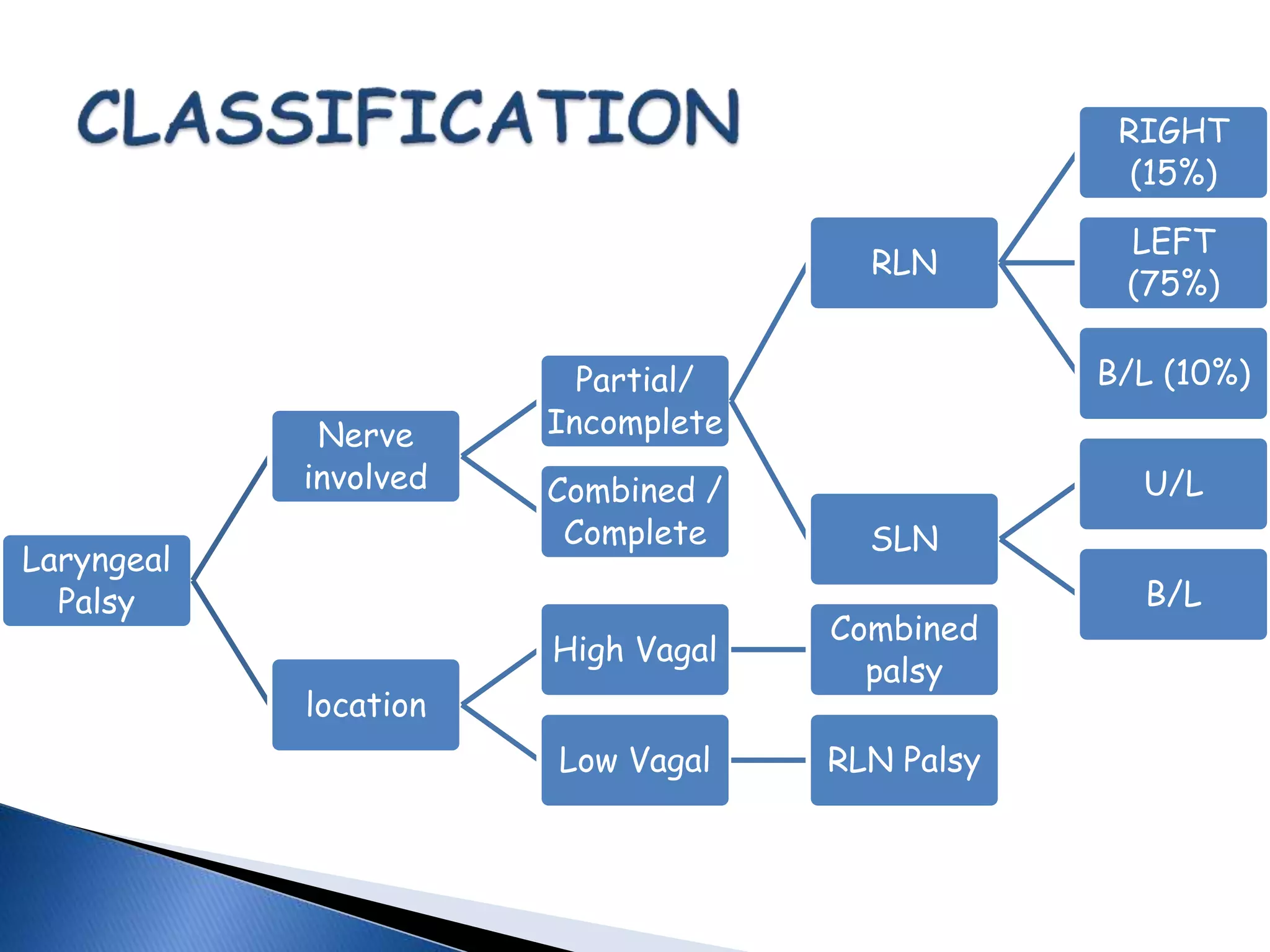
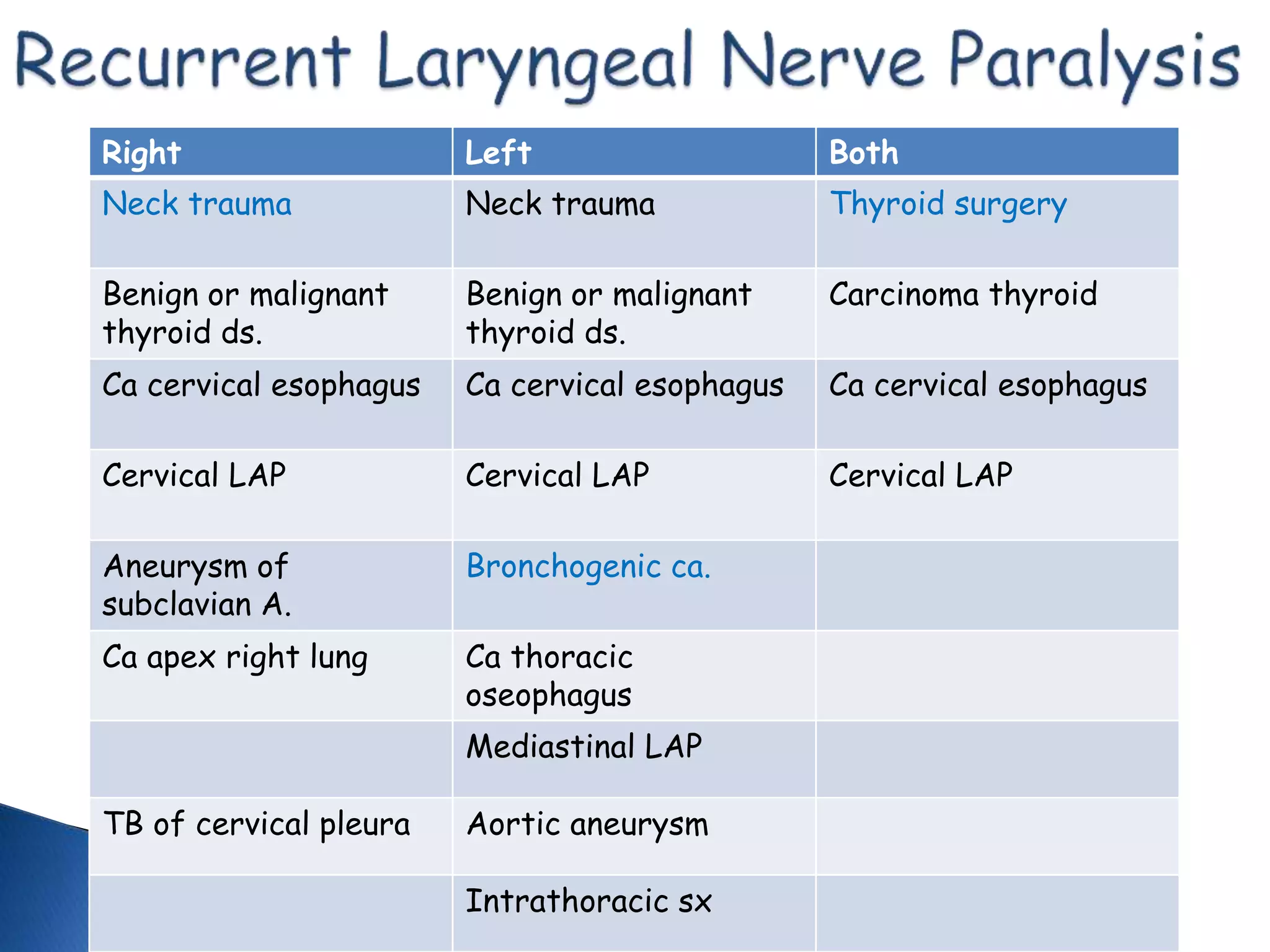
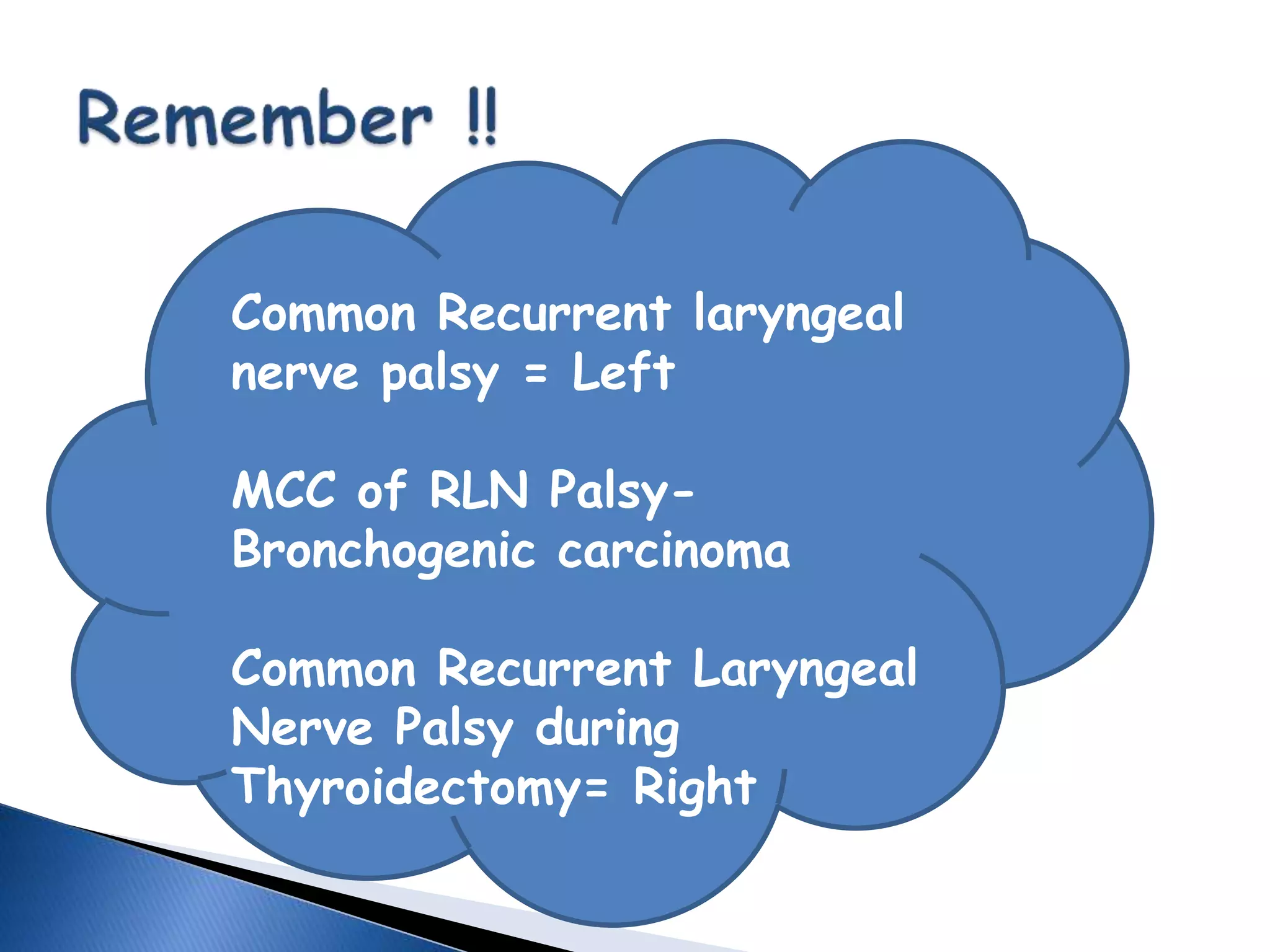
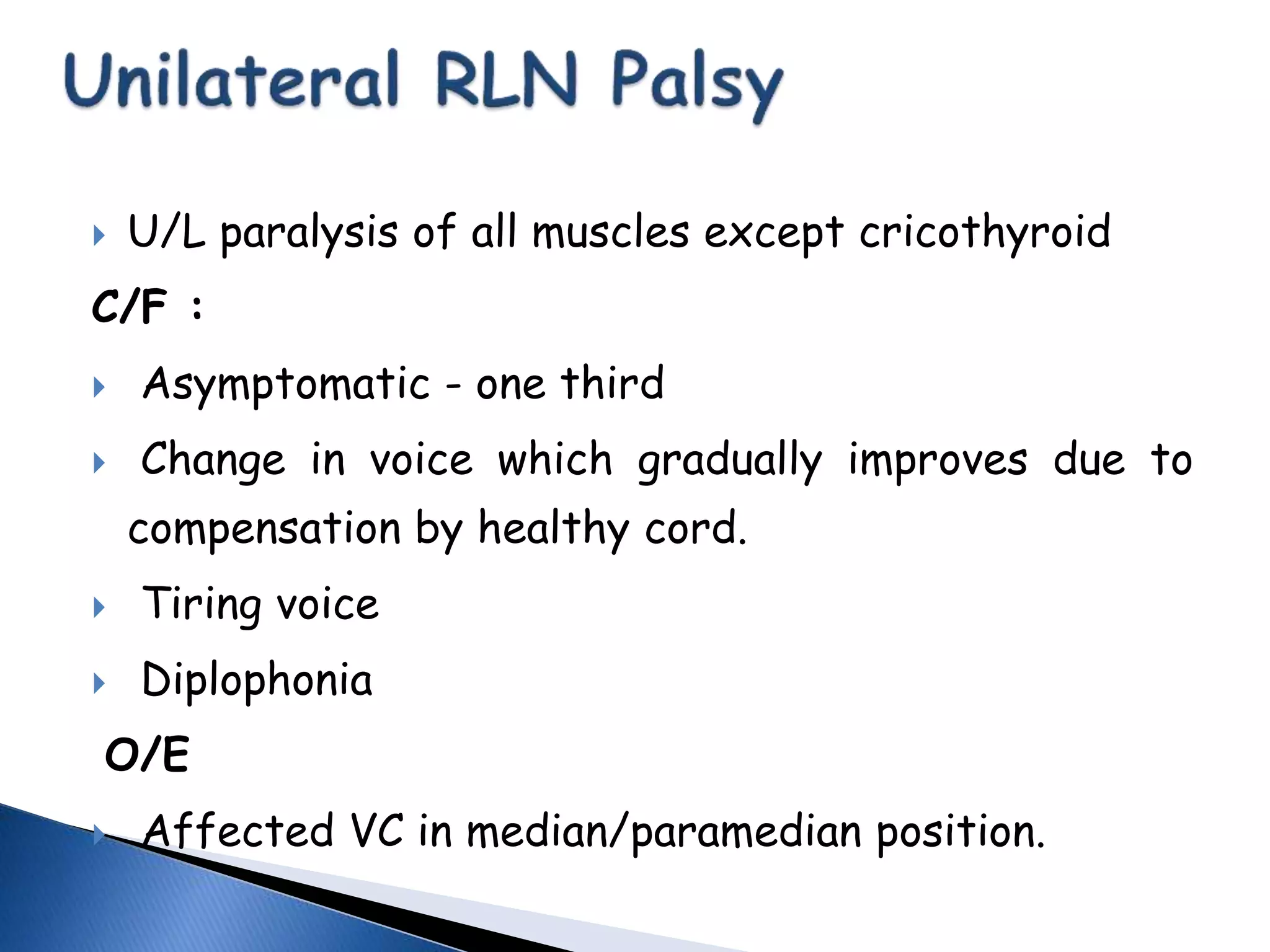
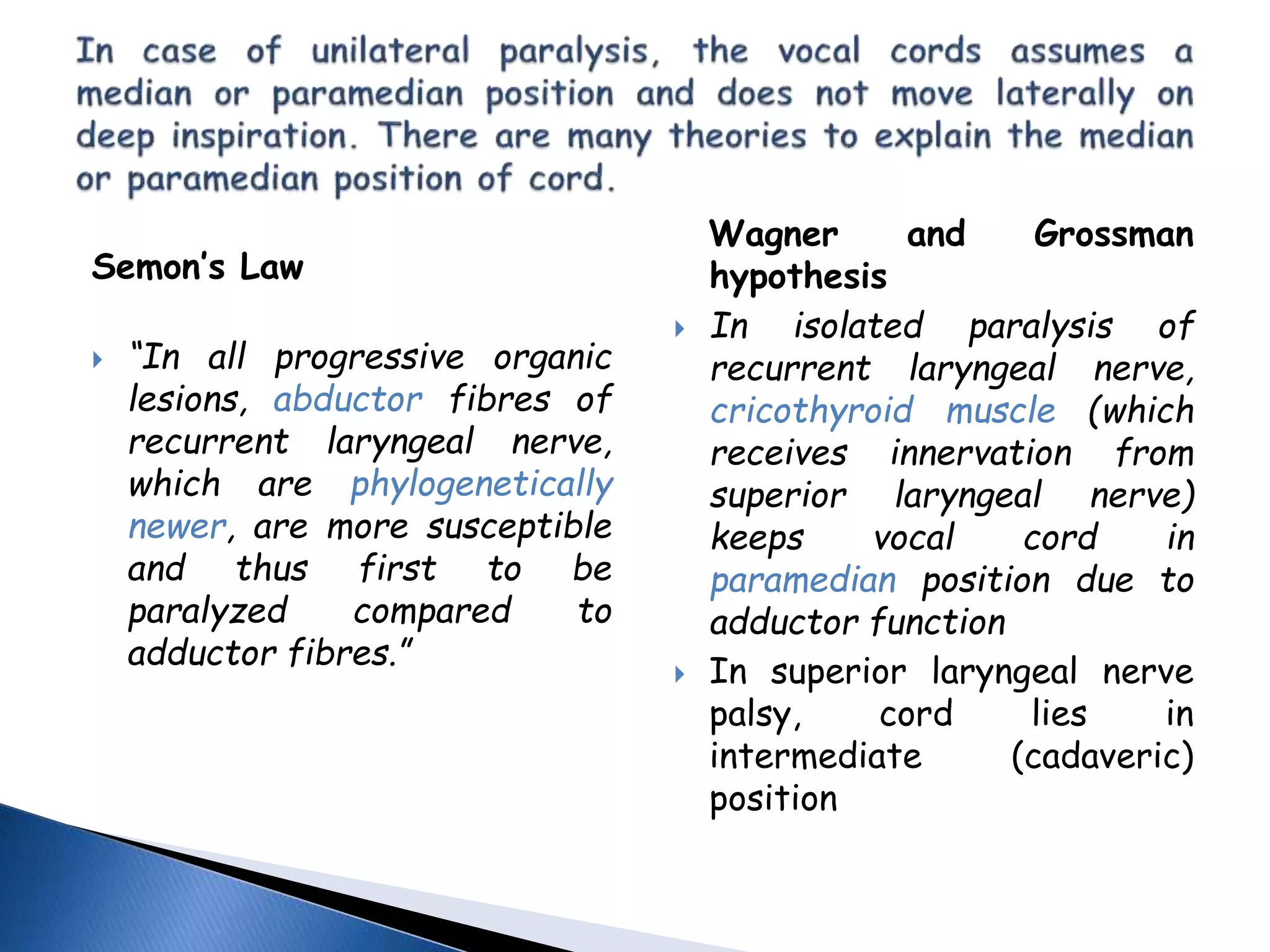
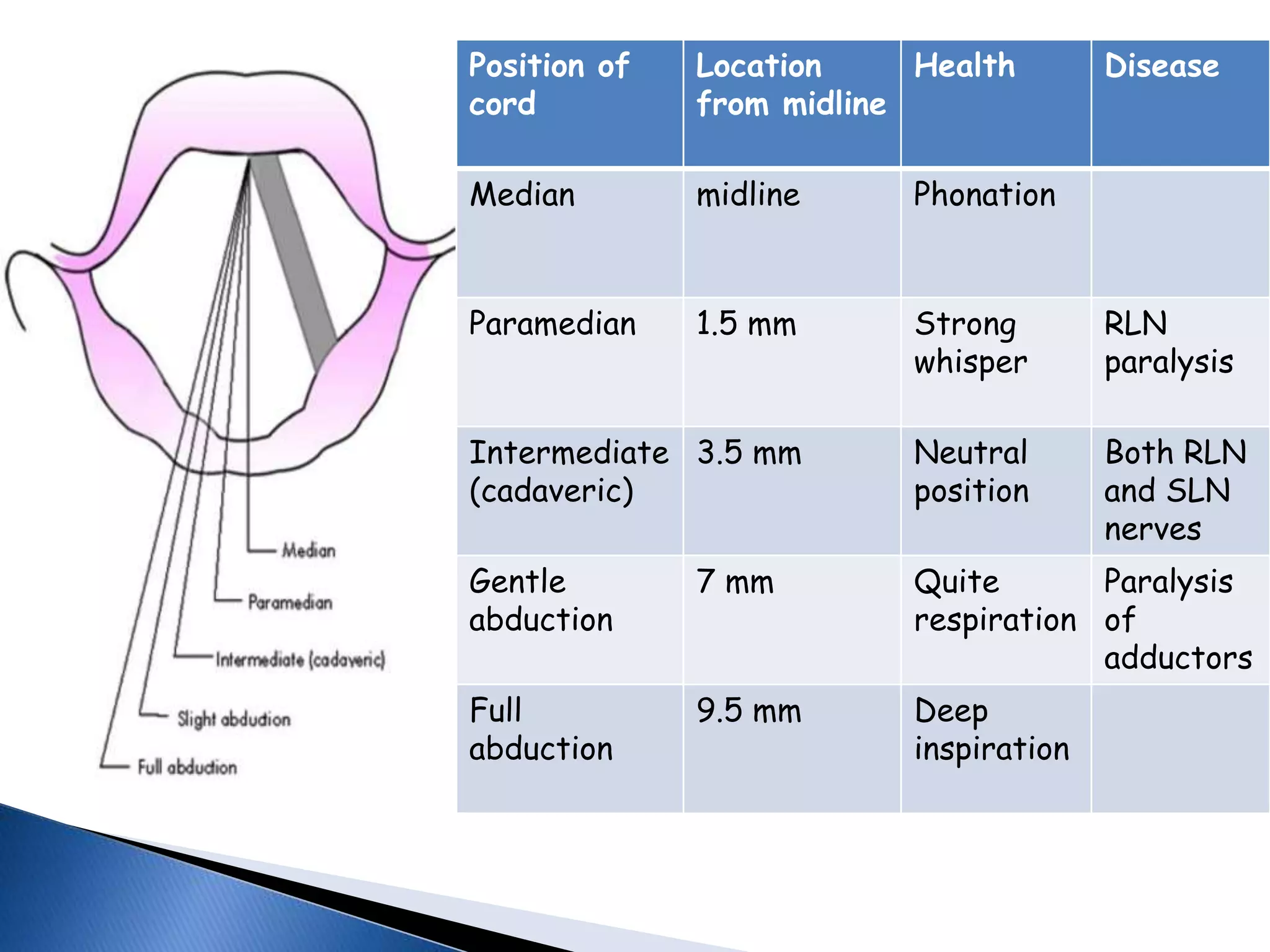
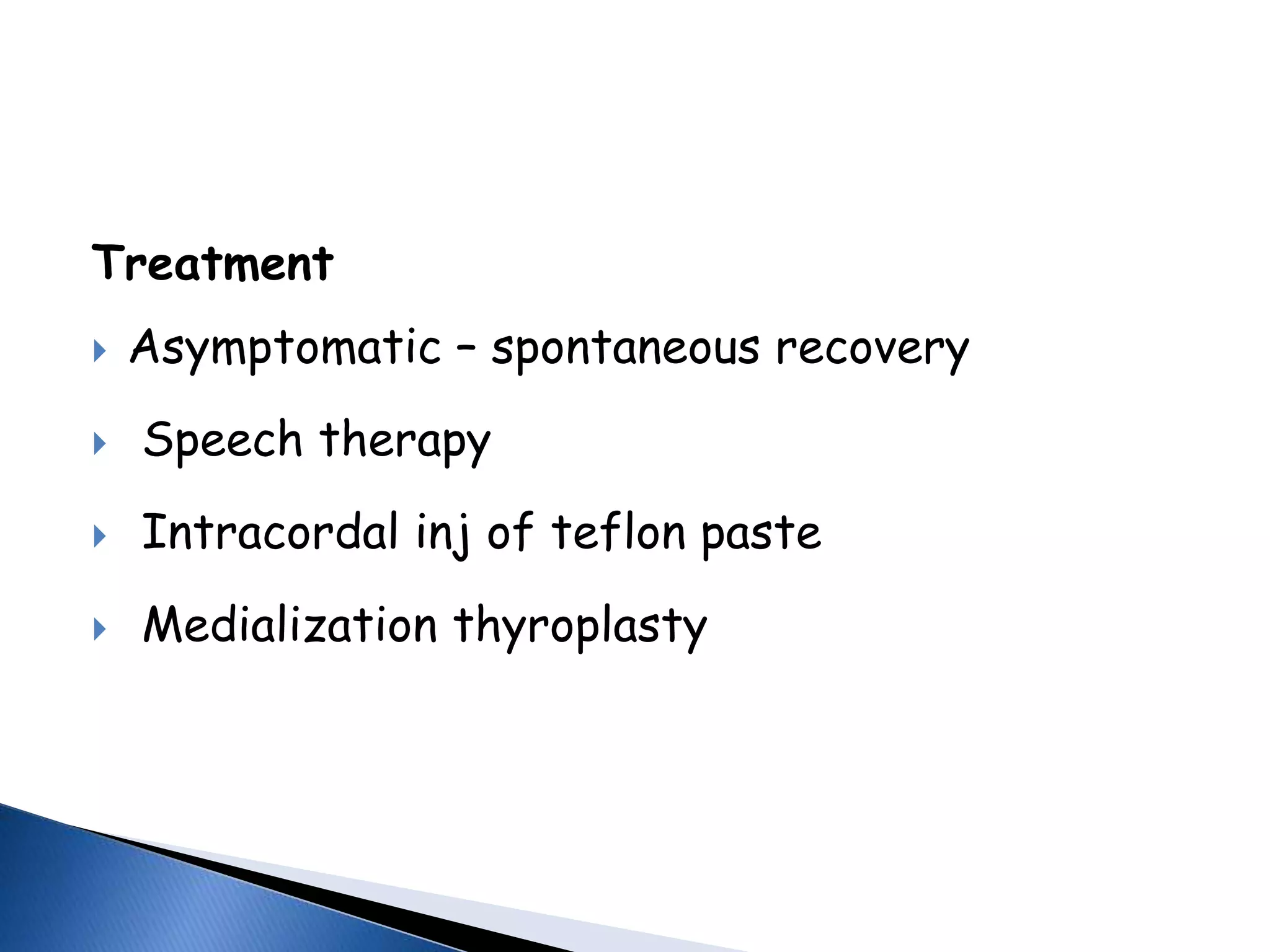
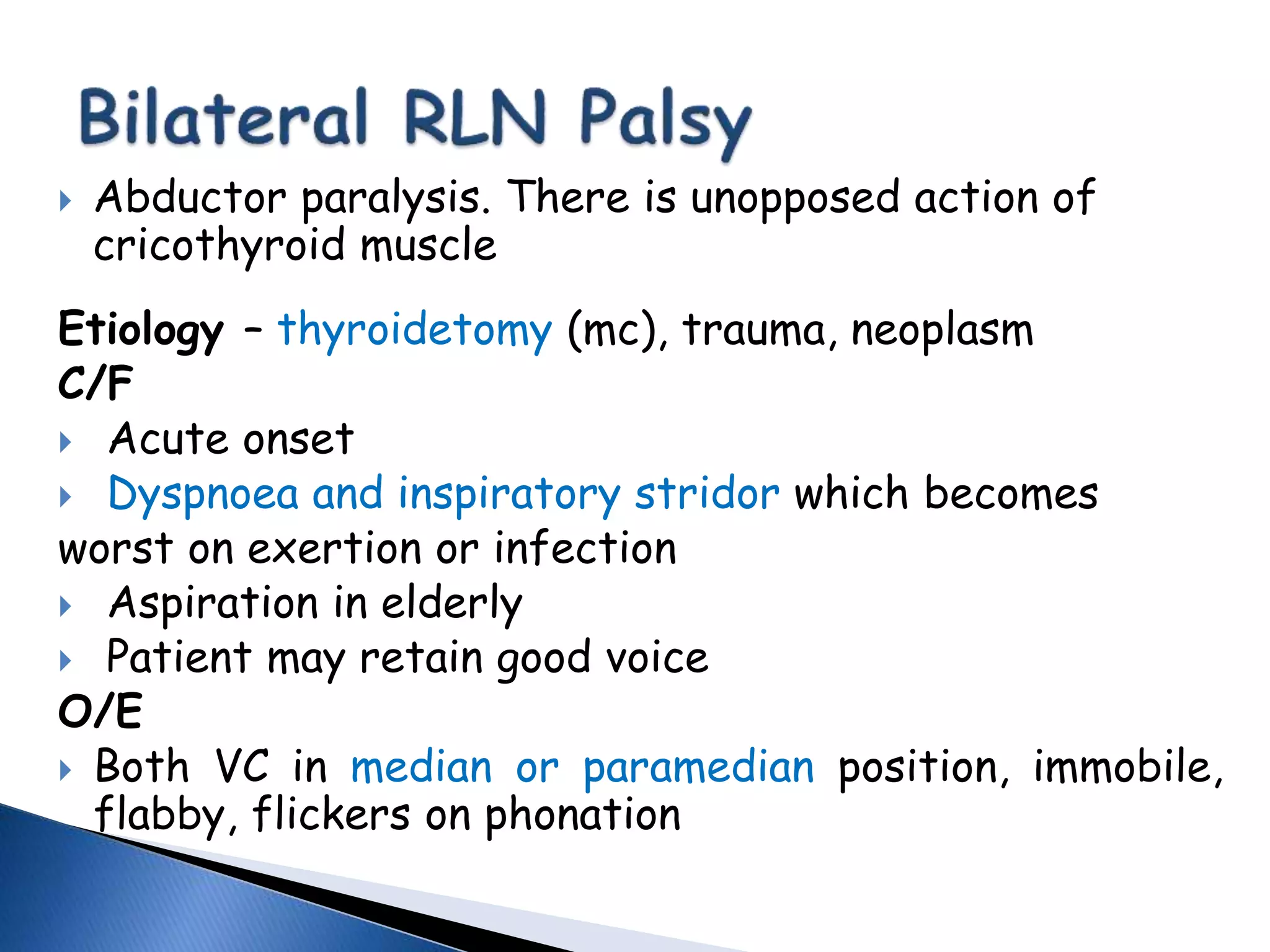
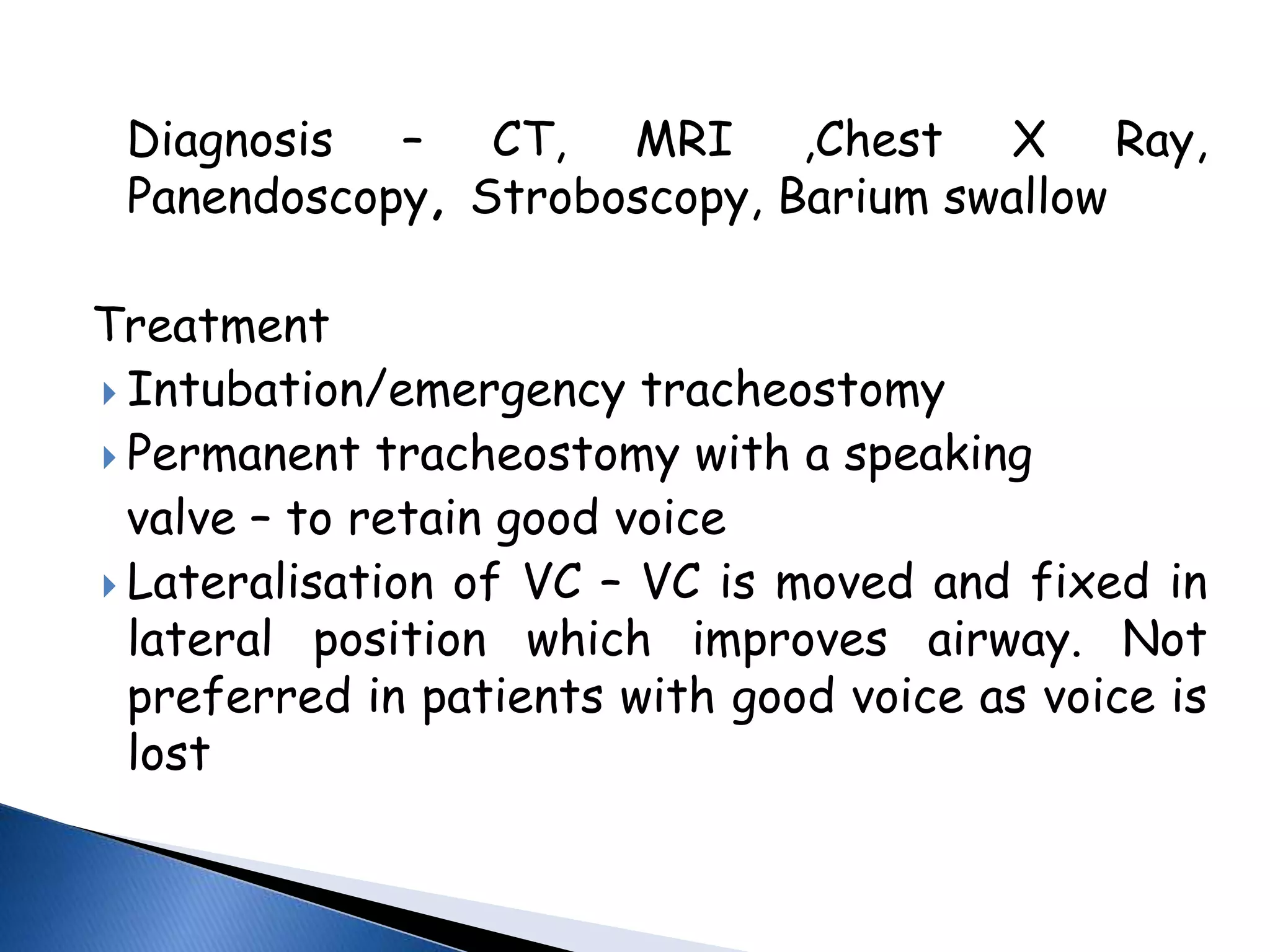
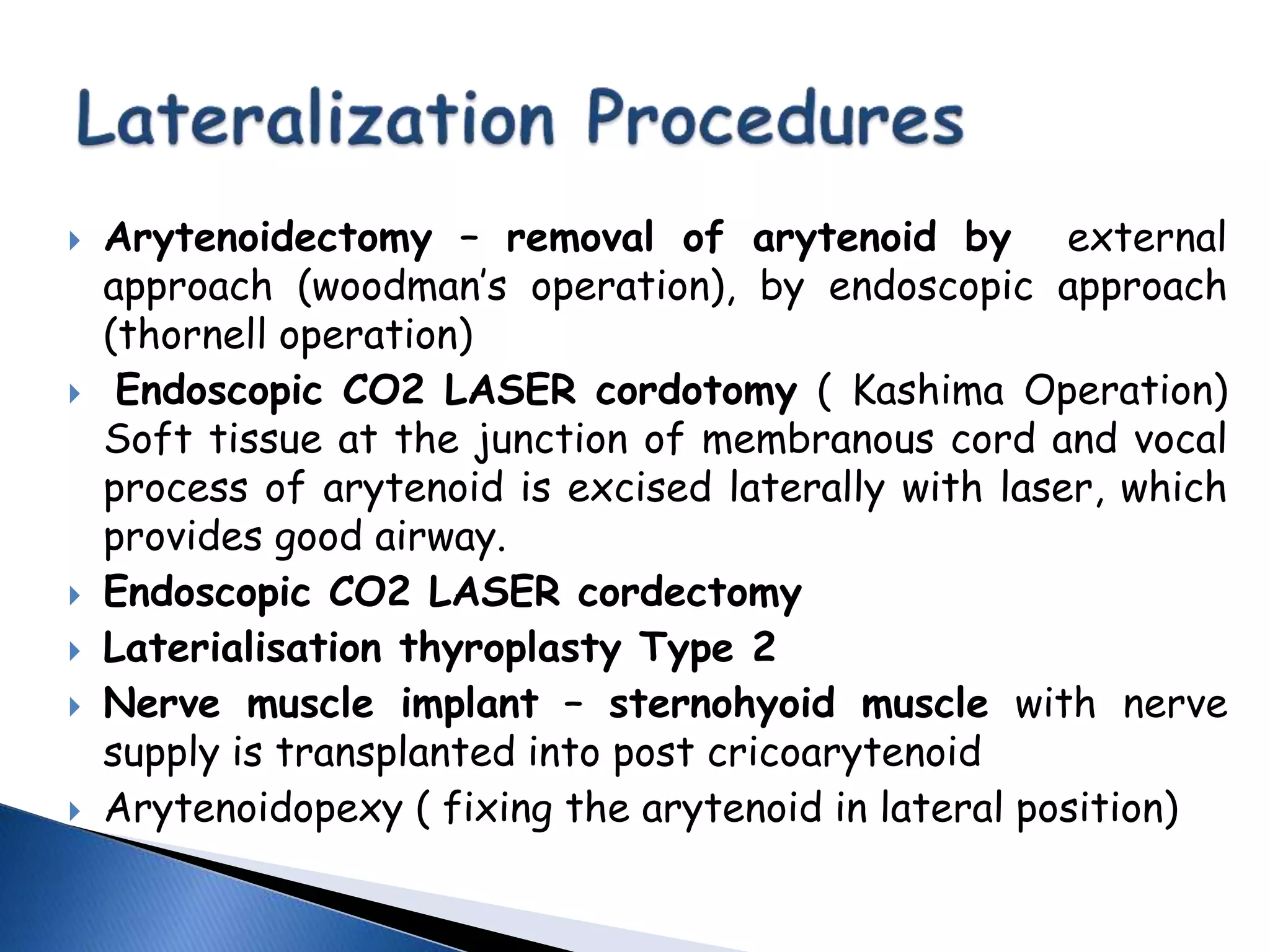
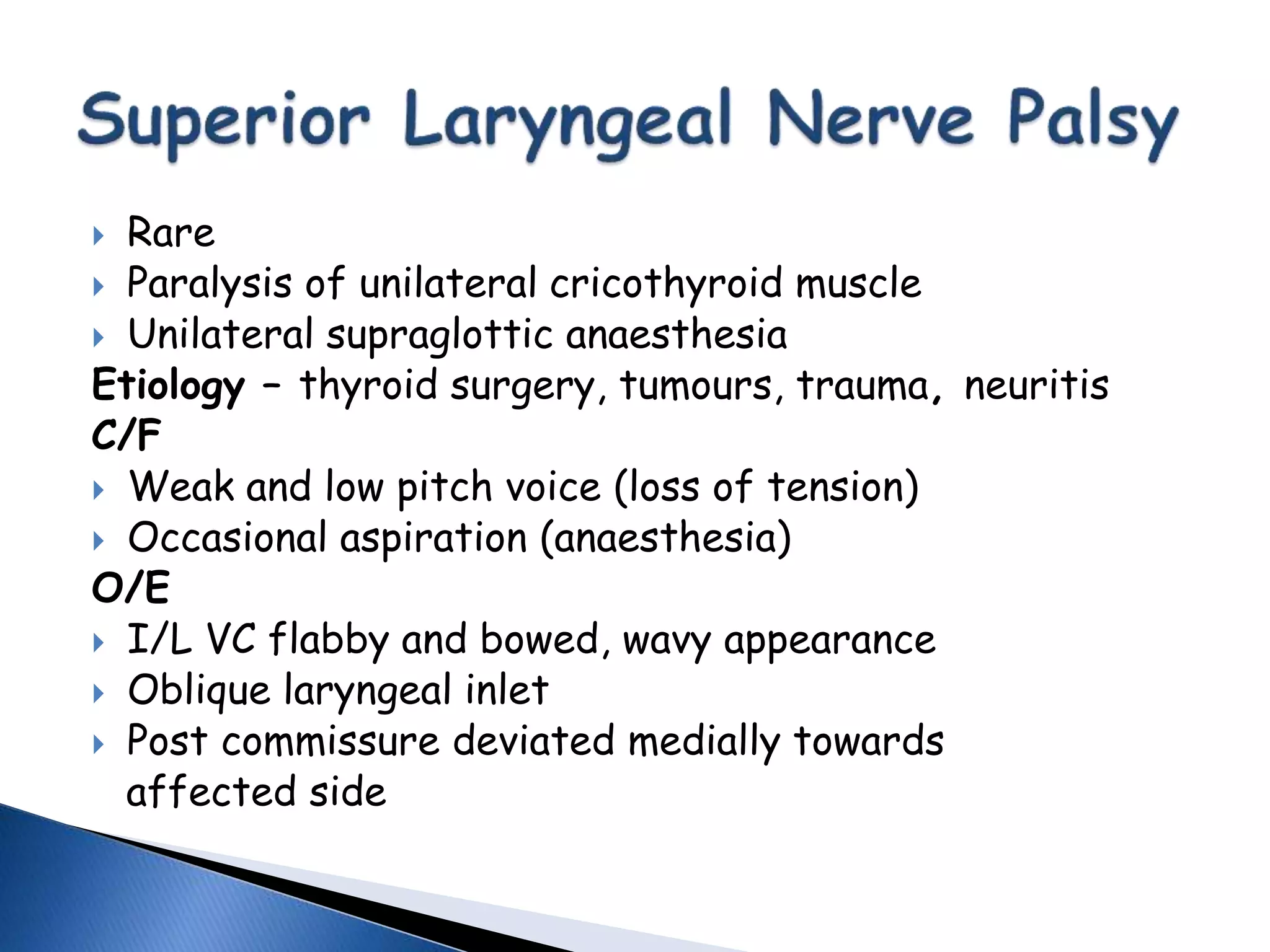
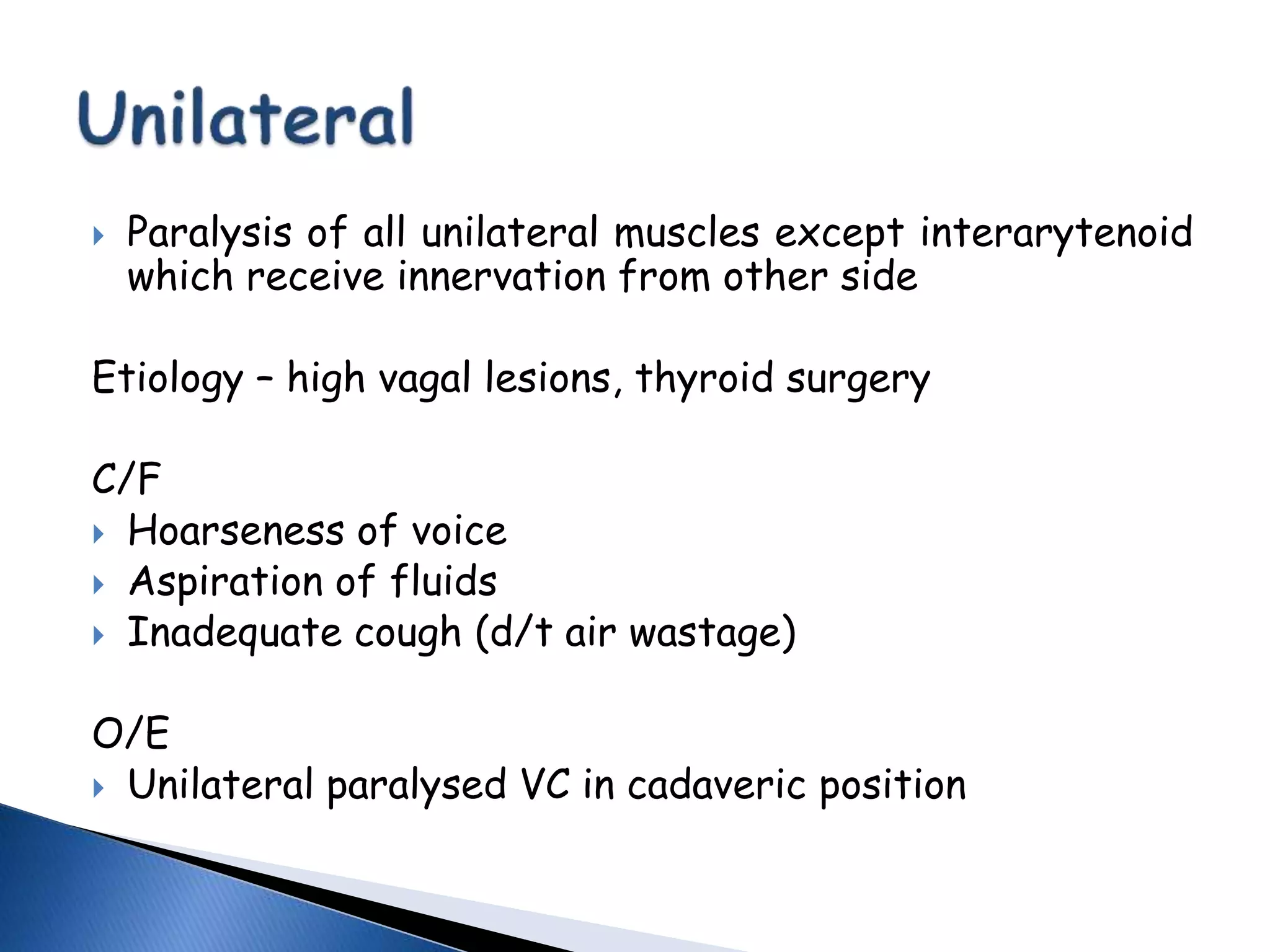
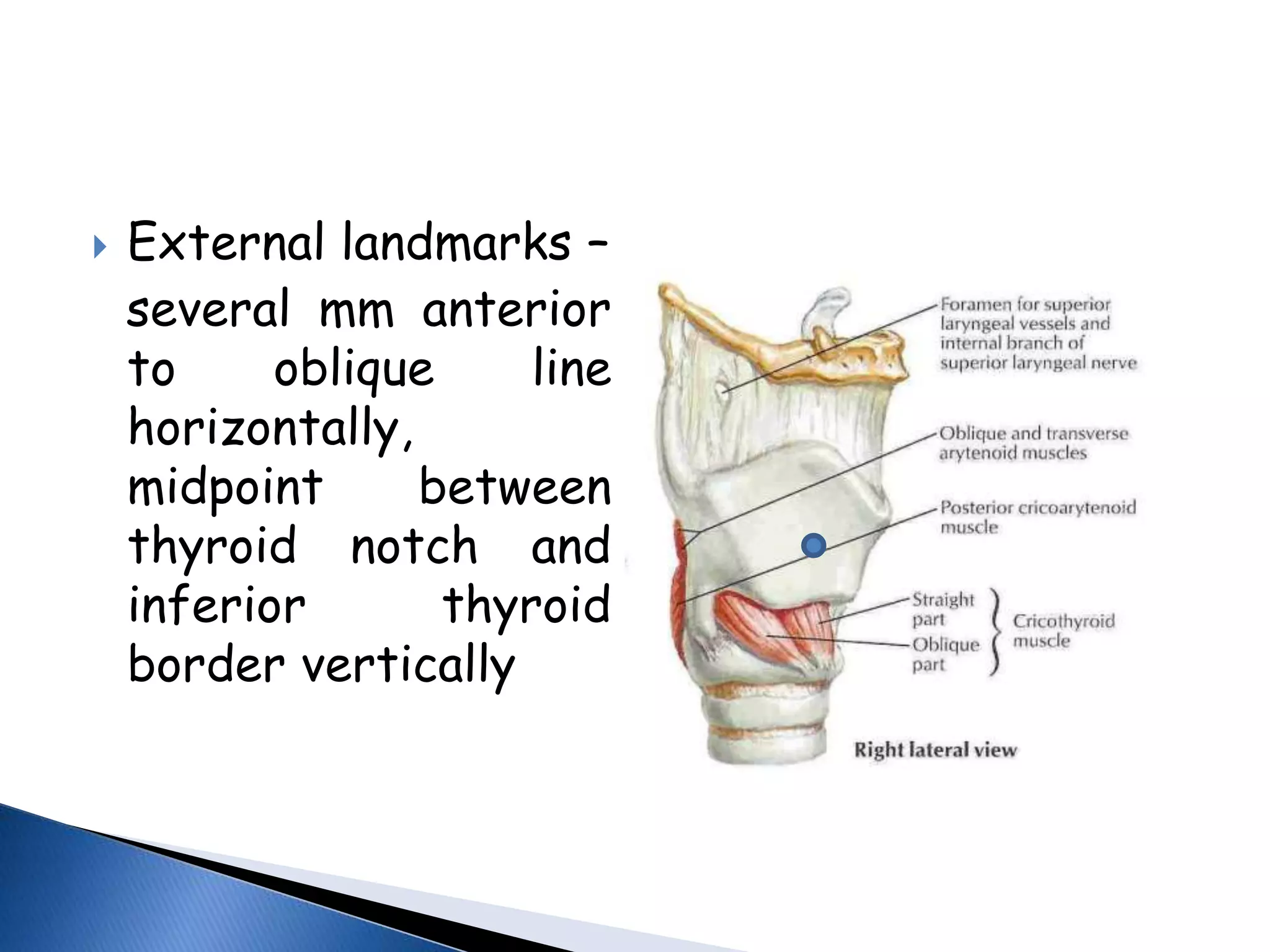
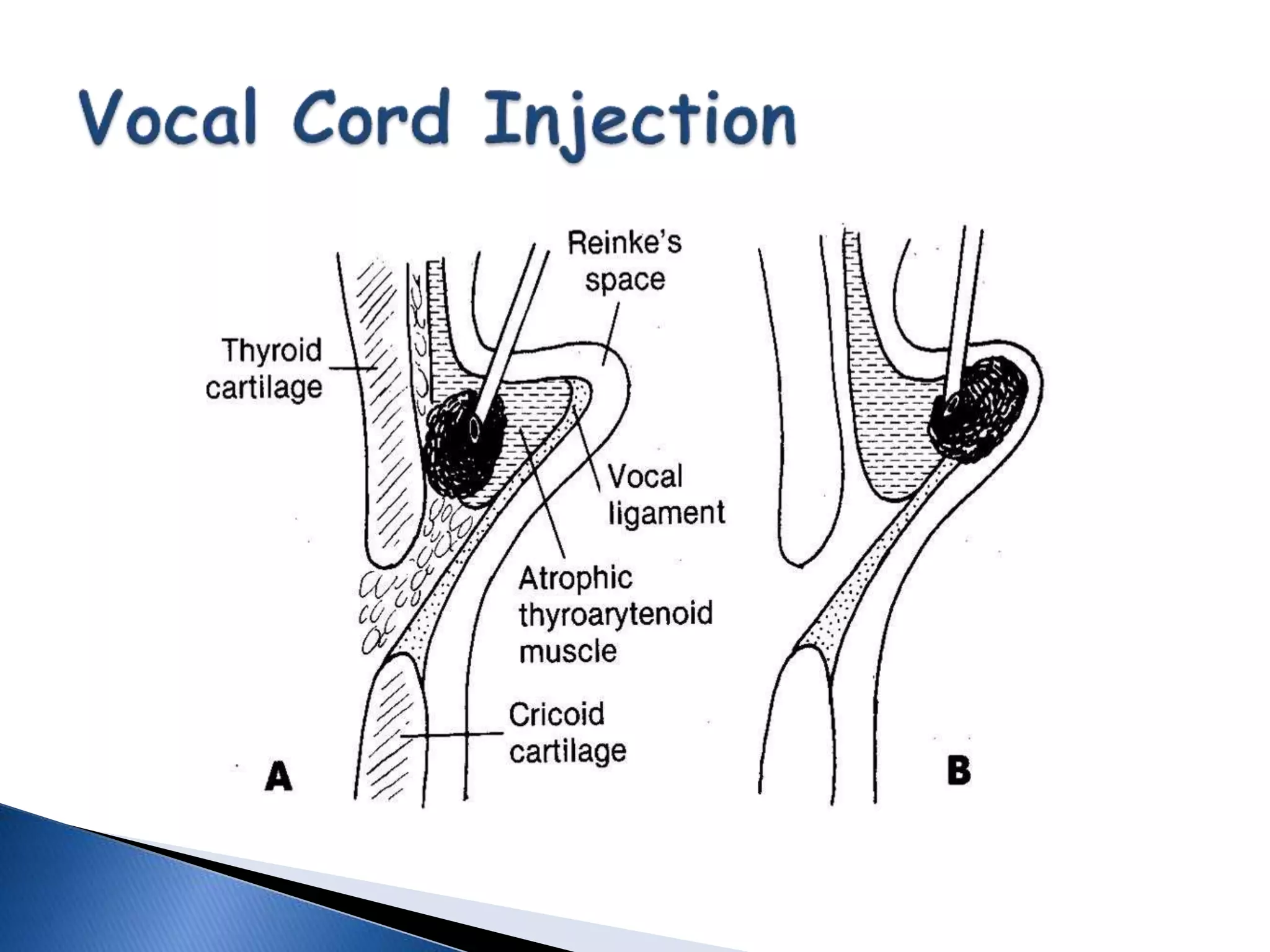
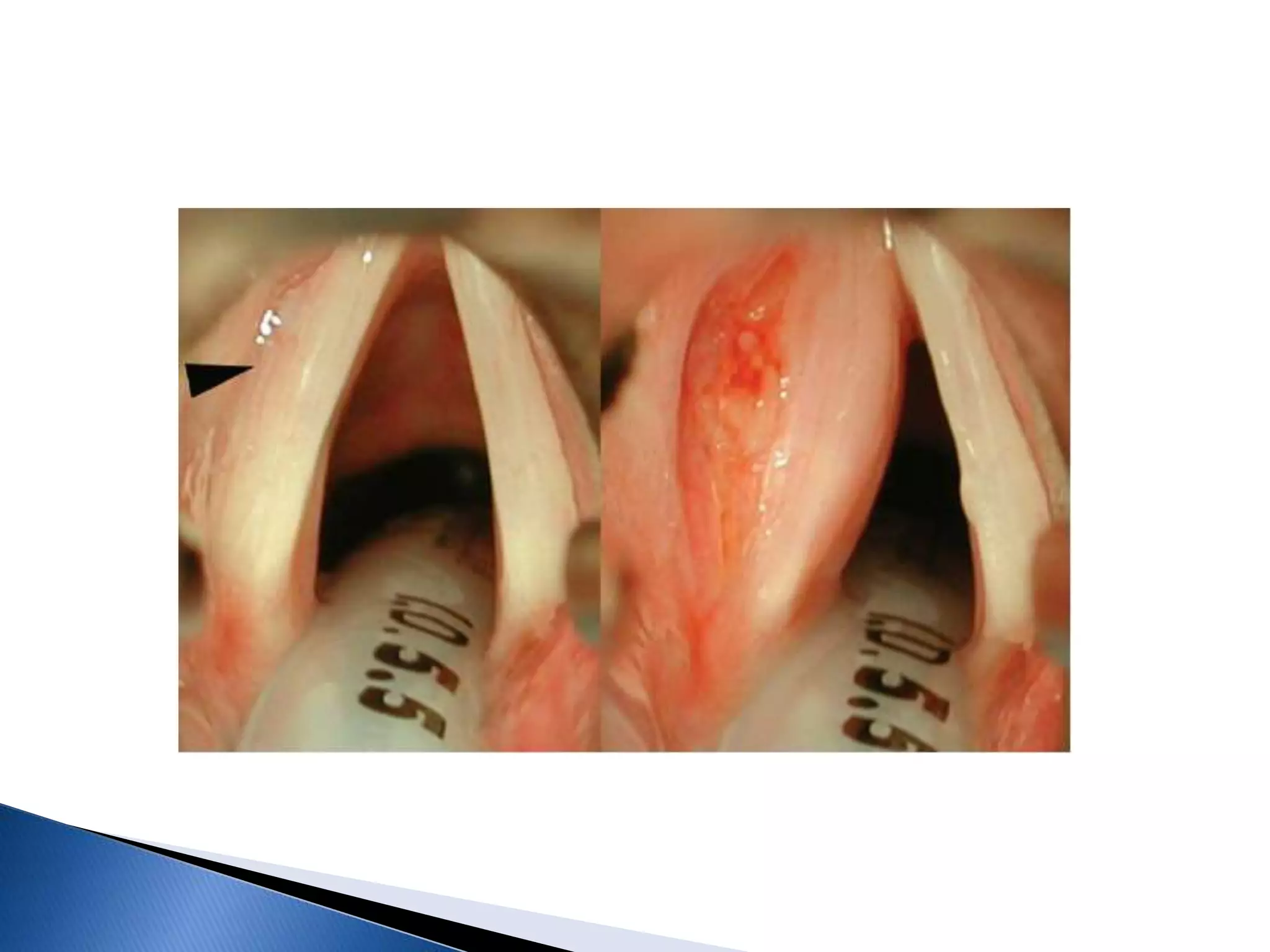
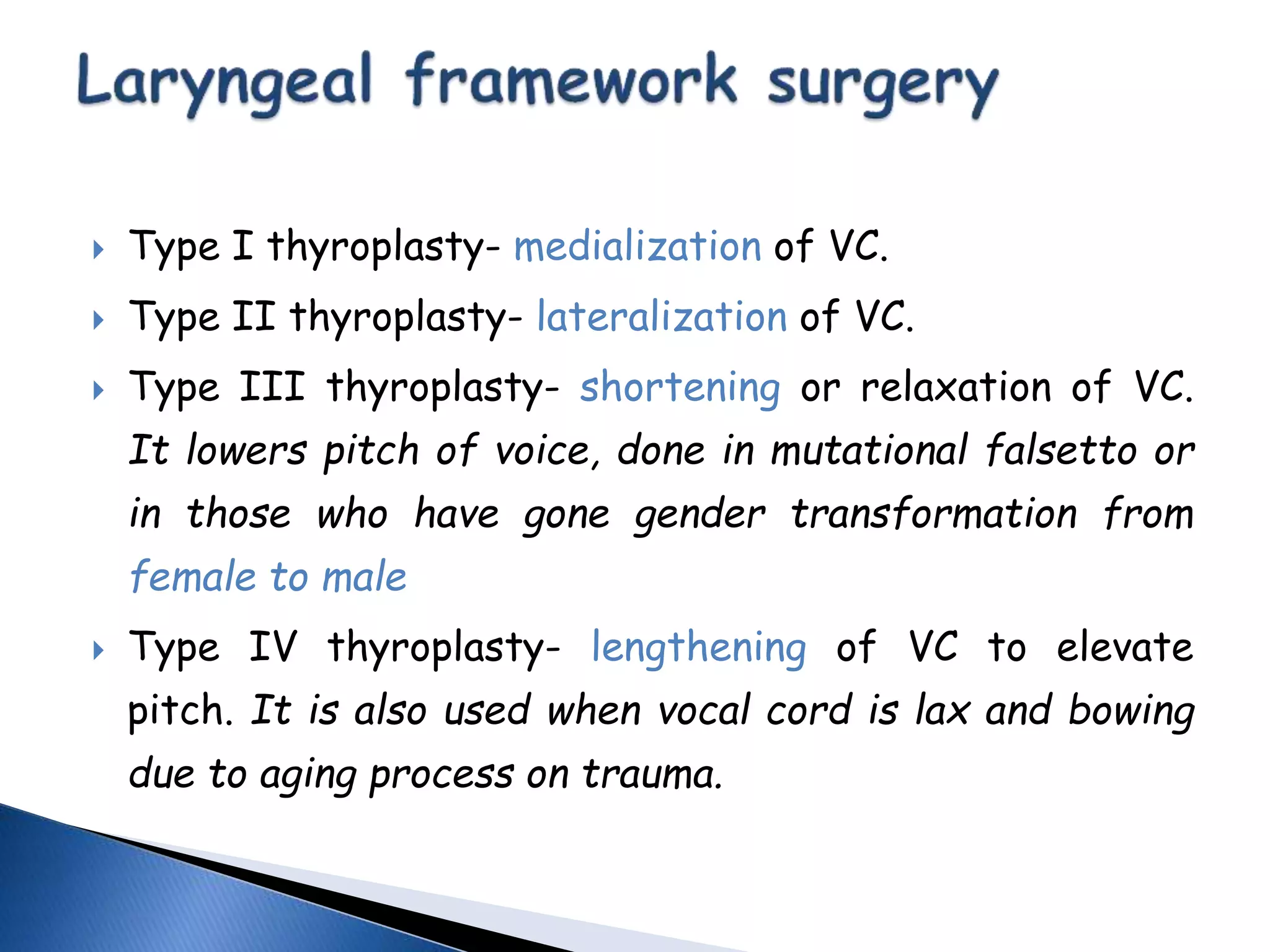
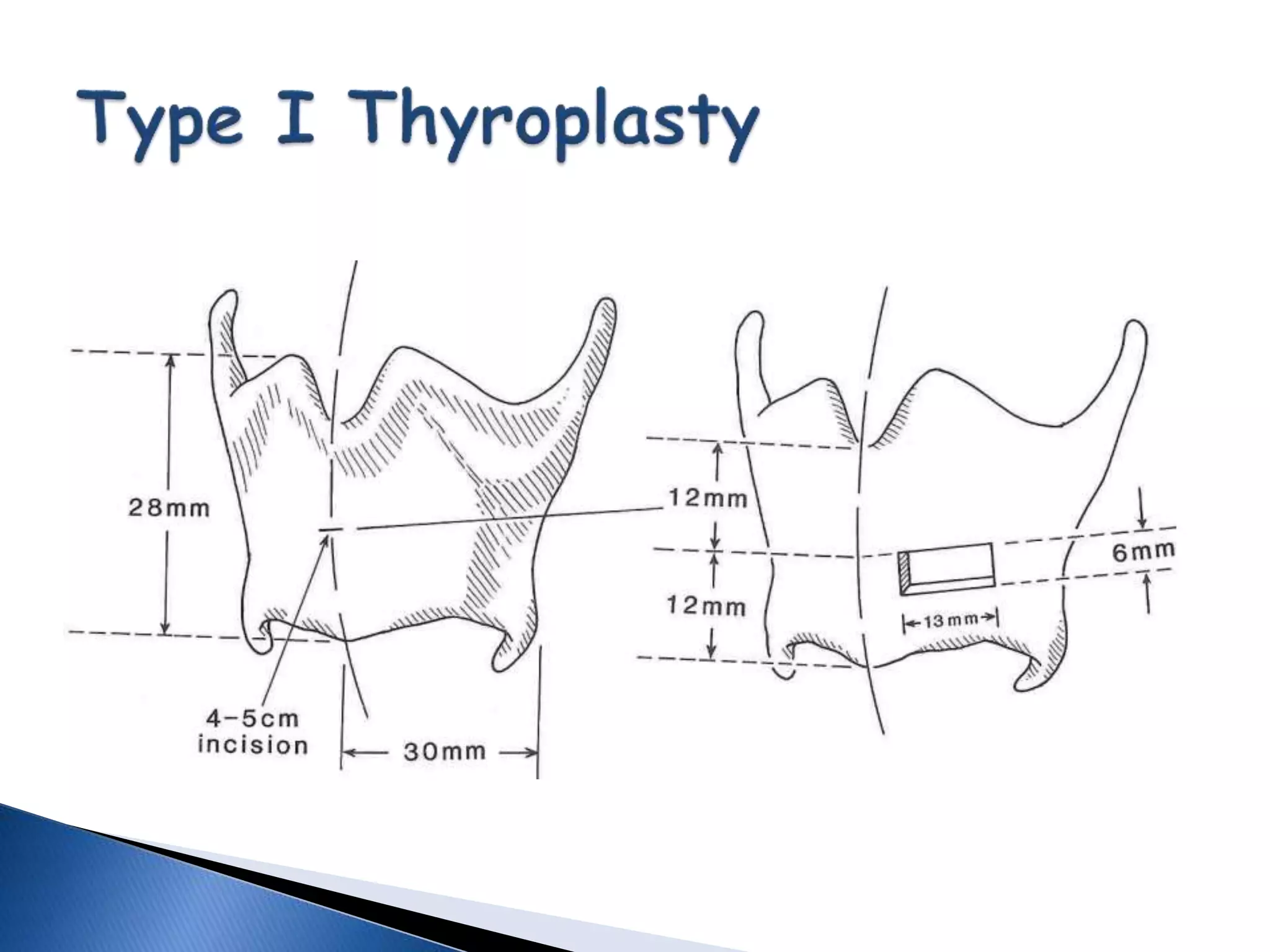
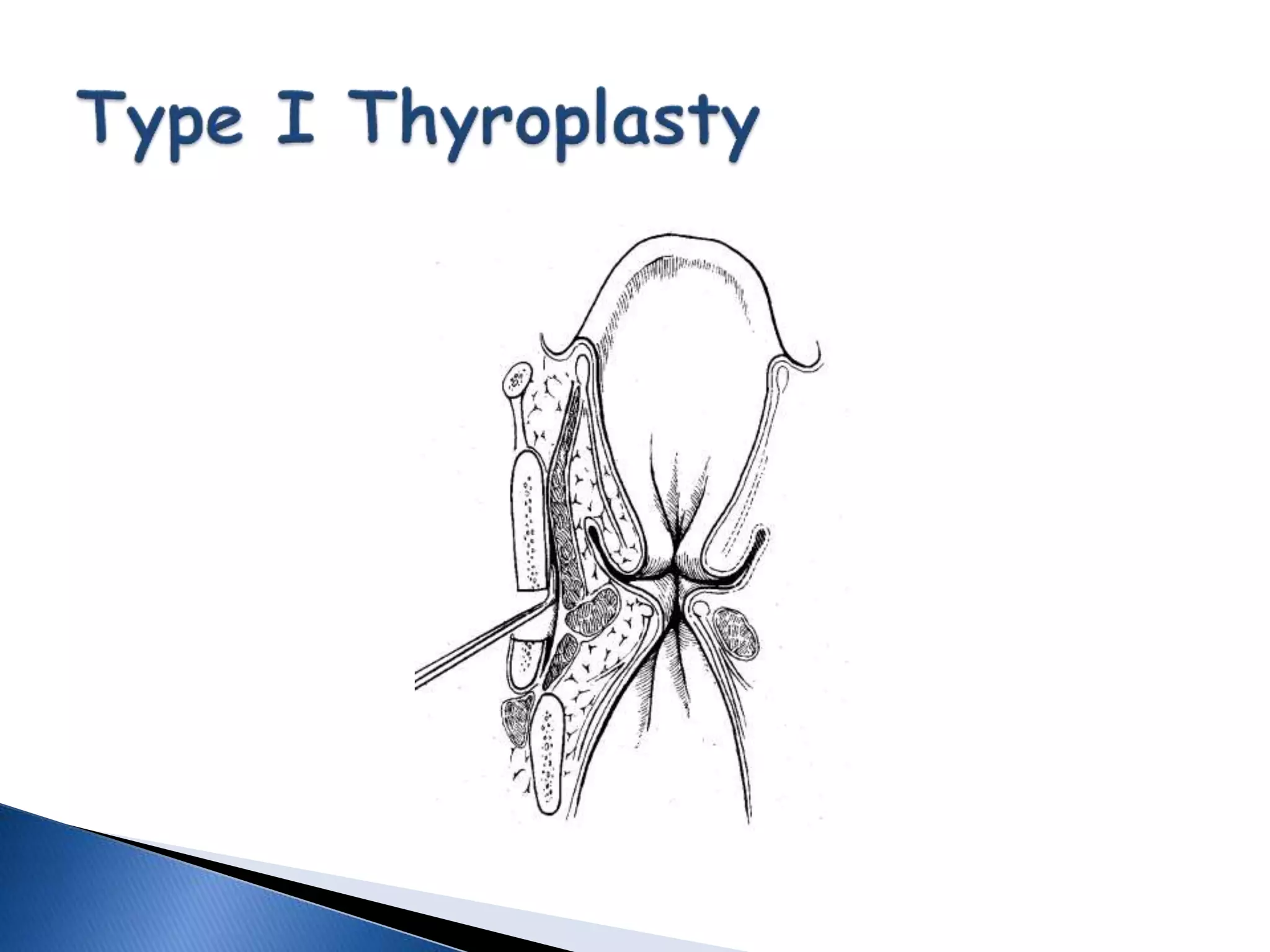
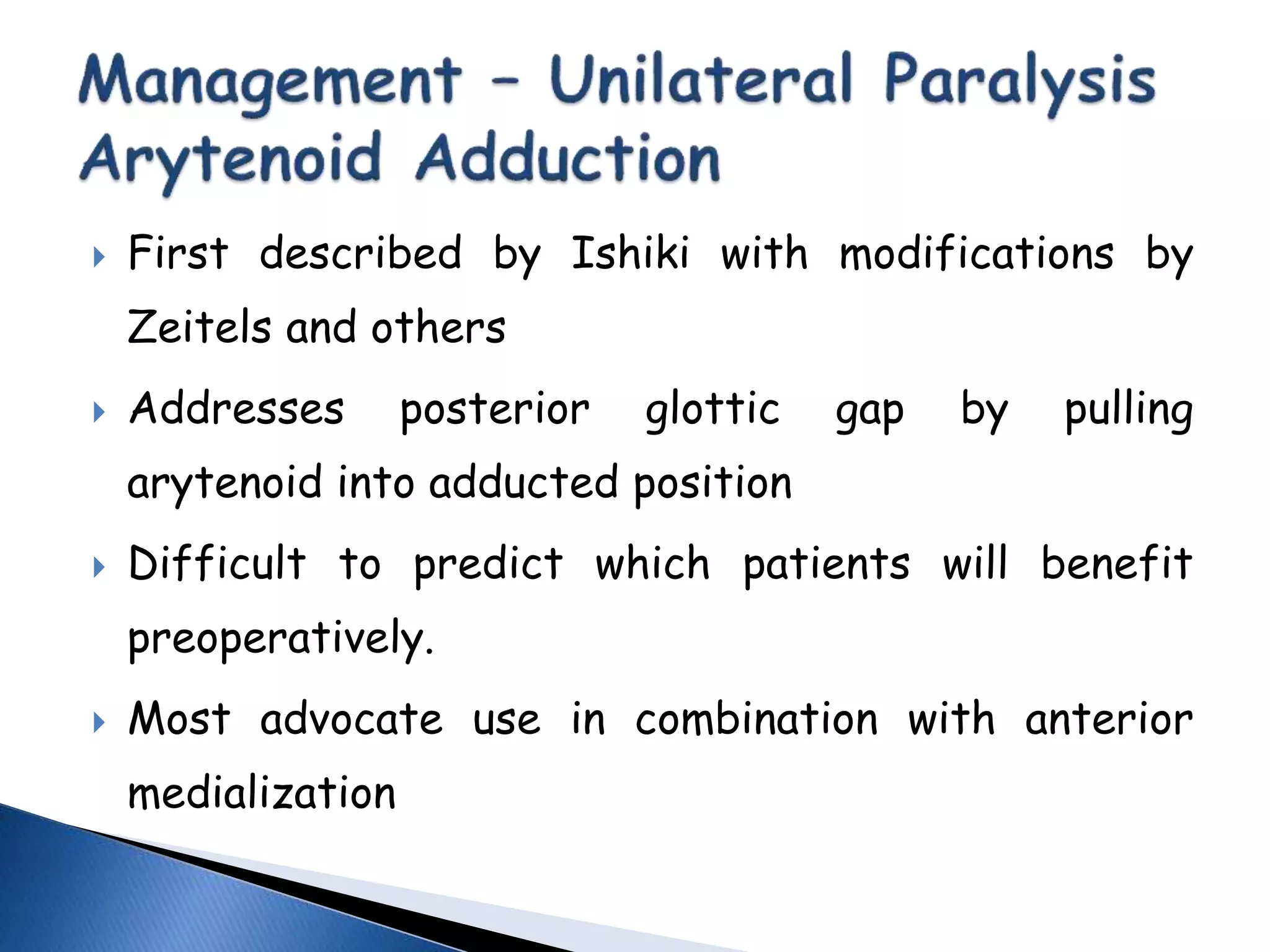
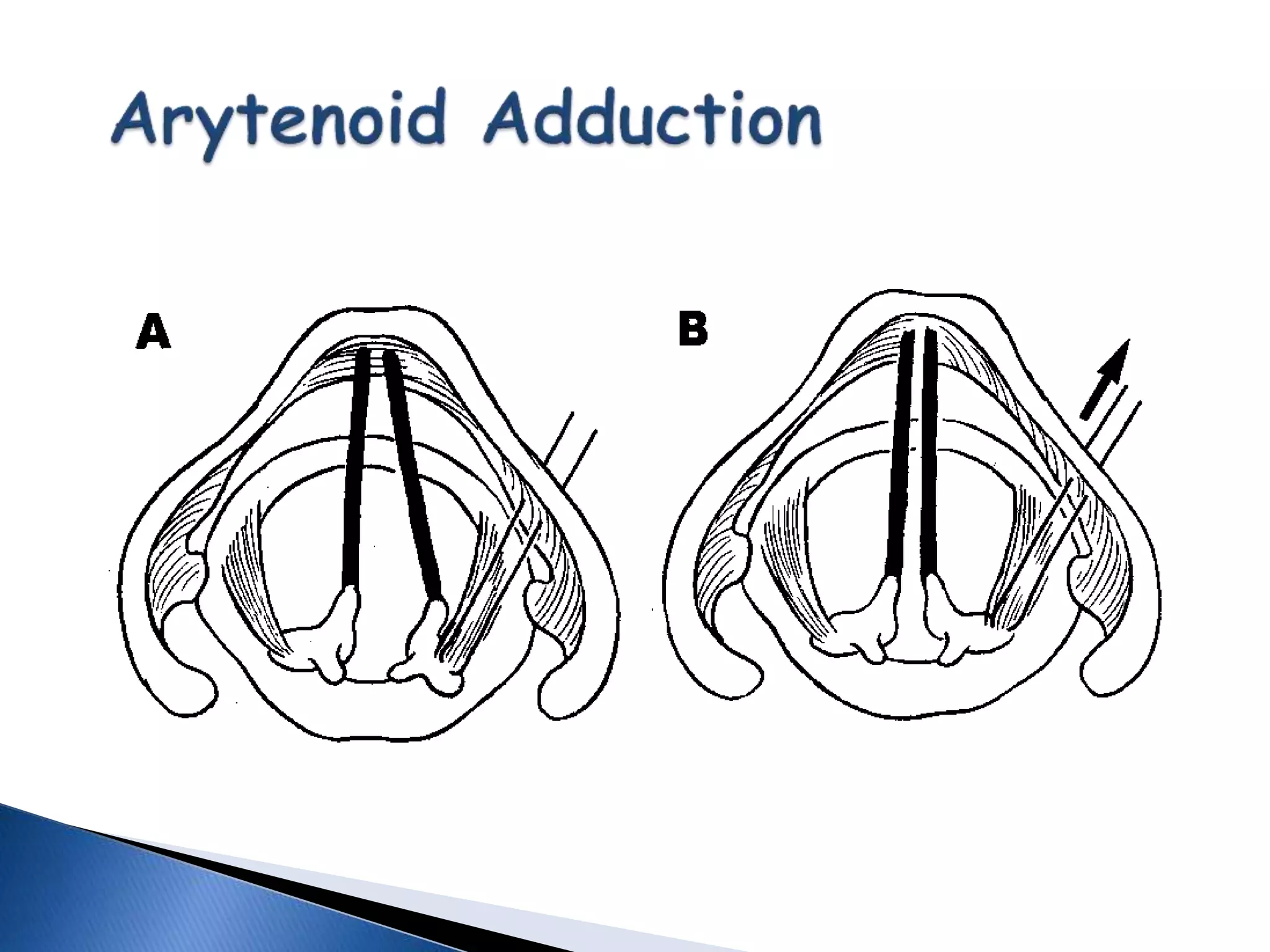
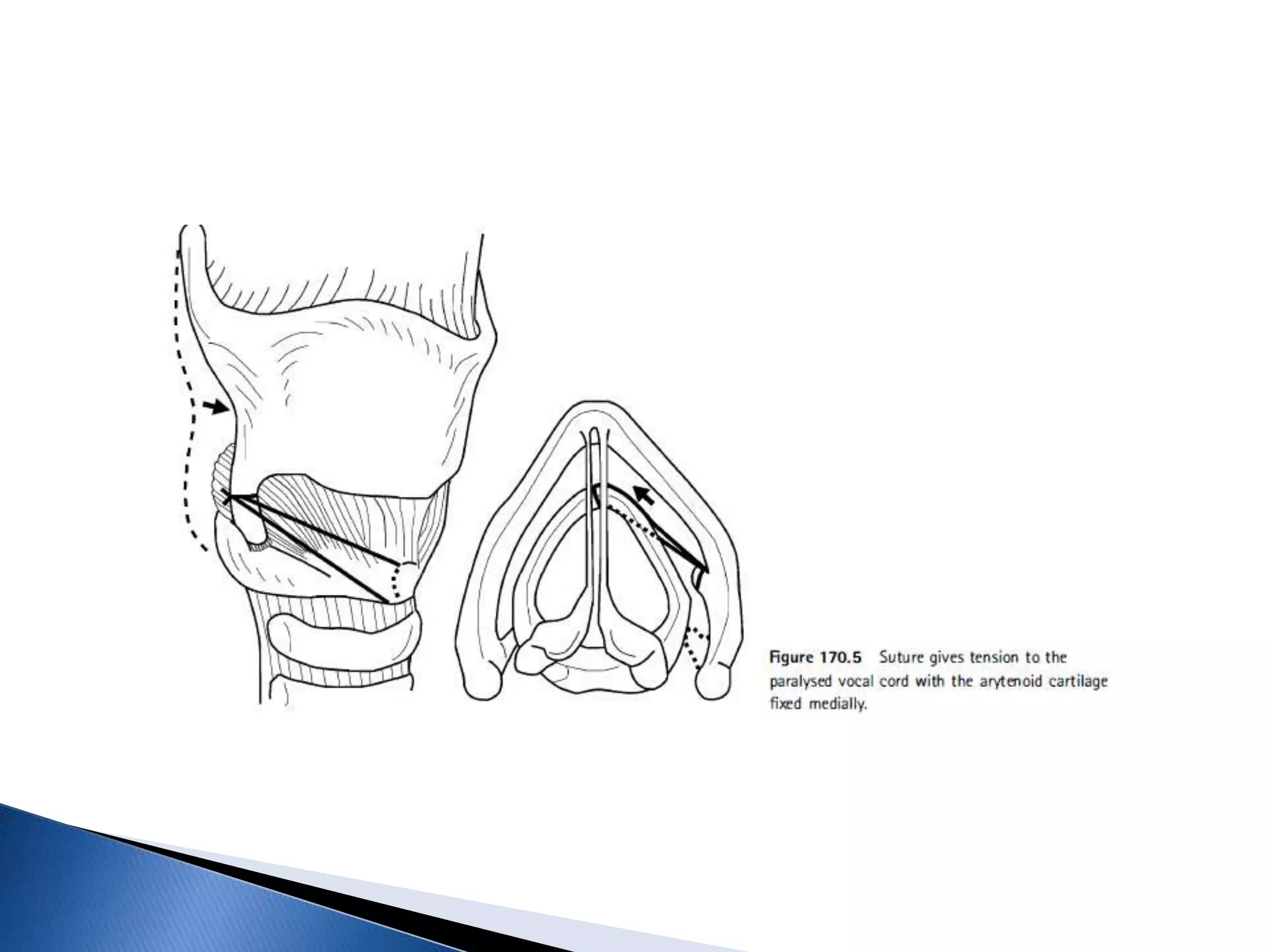
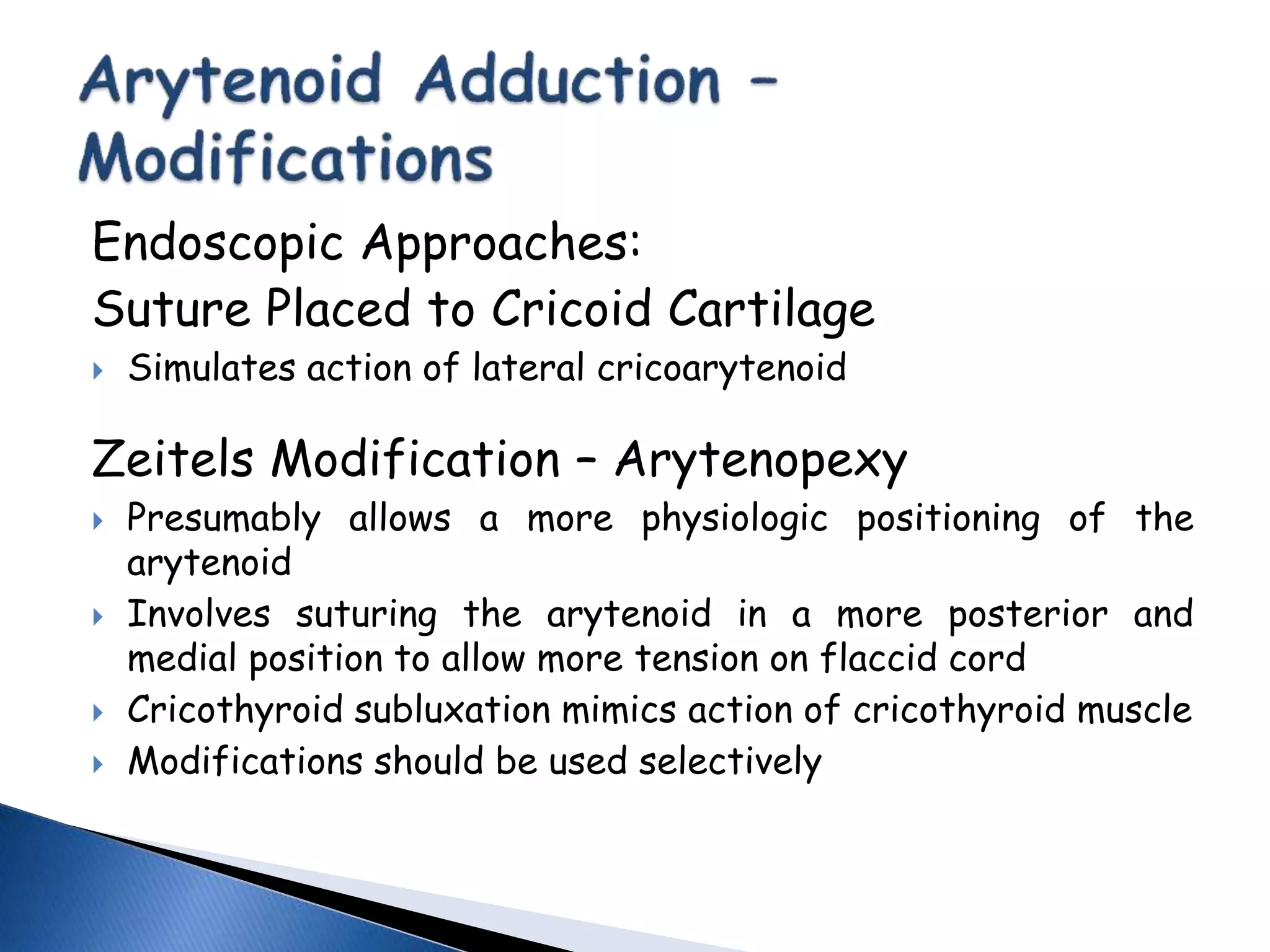
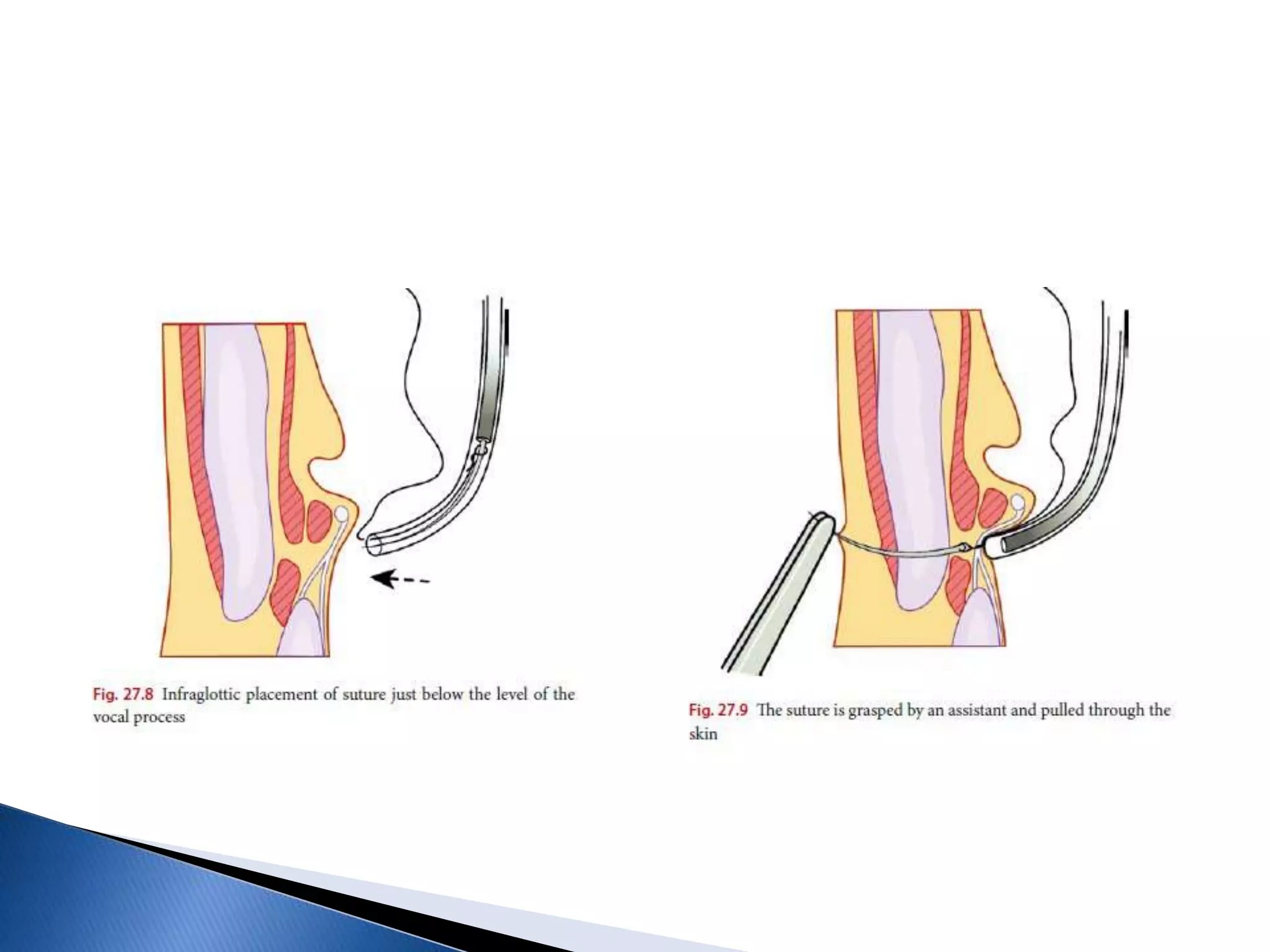
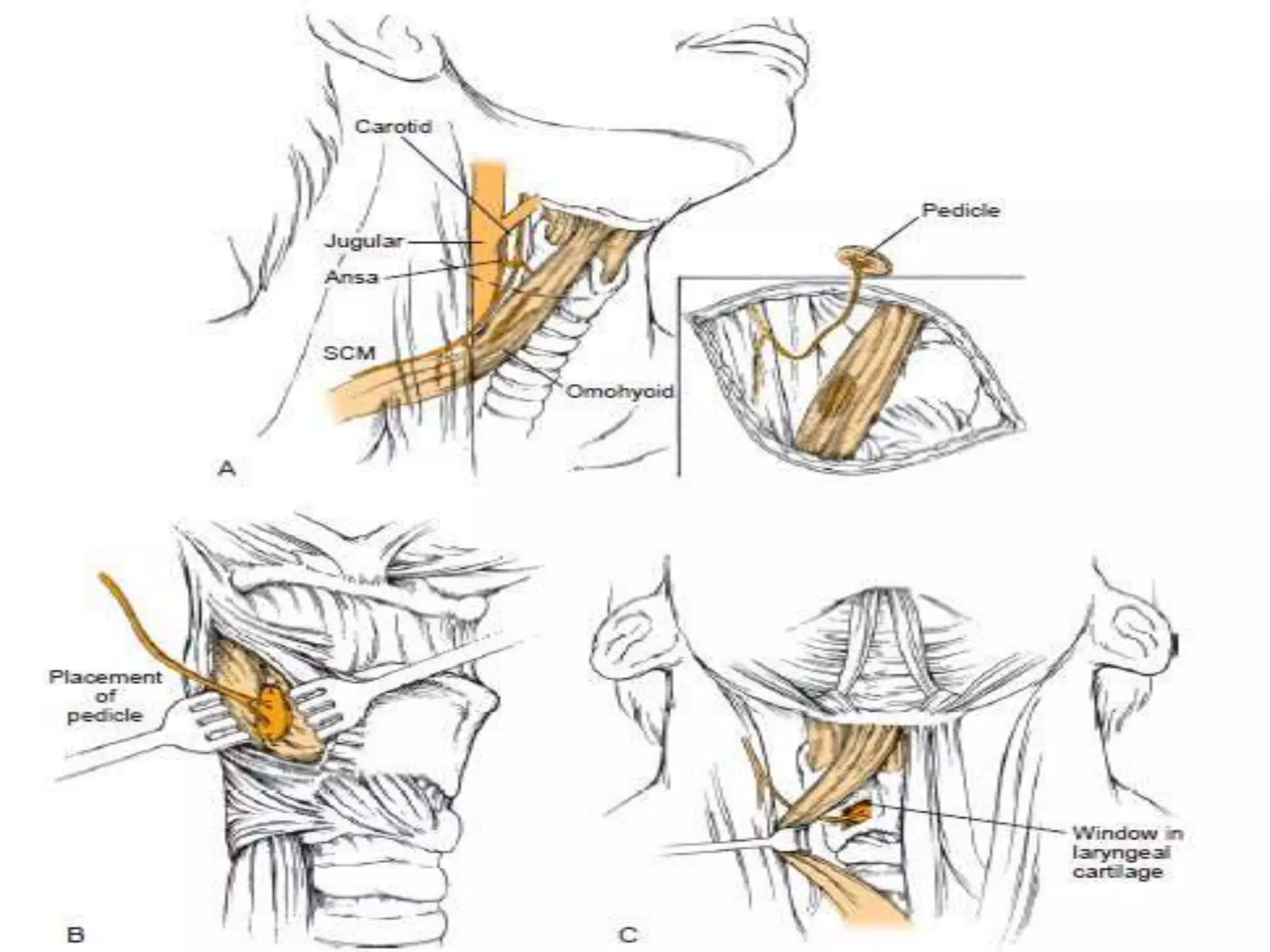
This document discusses the anatomy and nerve supply of the larynx. It describes the vagus nerve and its branches, including the recurrent laryngeal nerve. It discusses various types of laryngeal nerve palsies, including their causes, symptoms, examinations findings, and treatments. It provides details on the motor and sensory innervation of different parts of the larynx. Surgical procedures for treating laryngeal paralysis and techniques for vocal fold injection are also summarized.