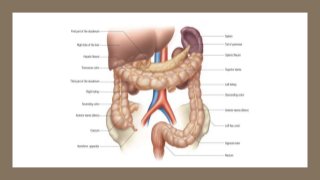
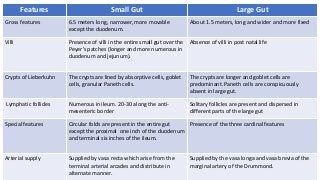
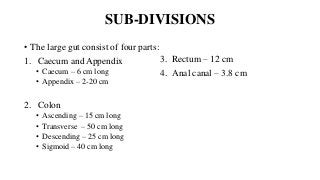
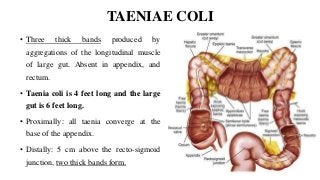
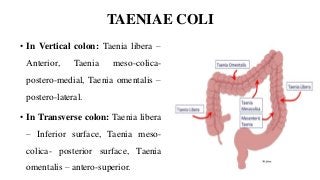
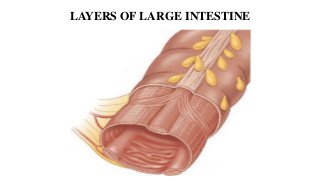
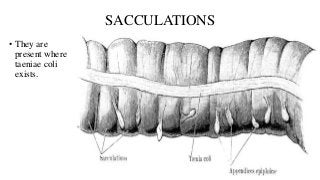
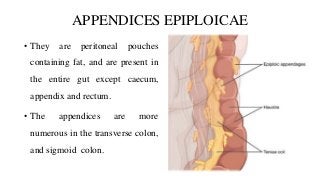
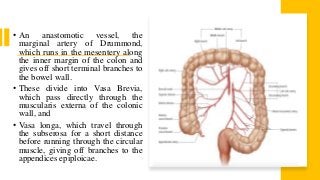
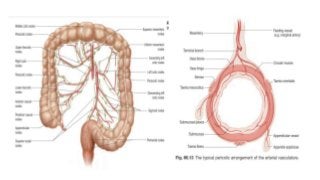
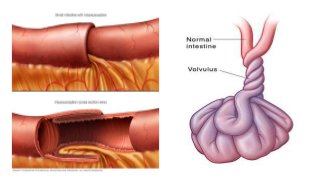
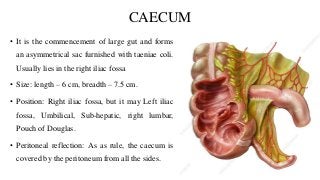
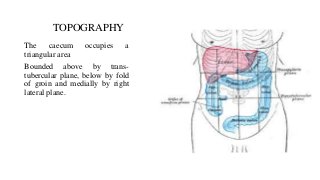
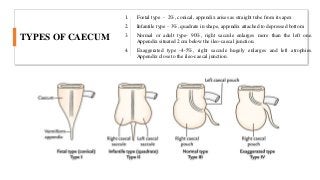
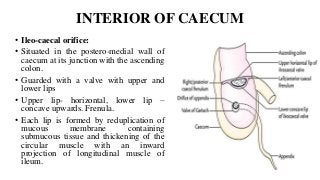
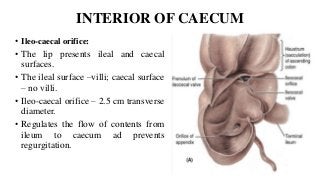
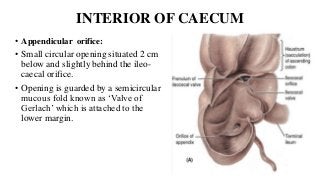
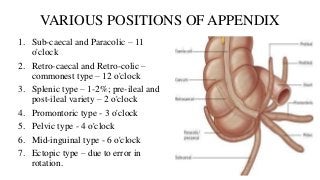
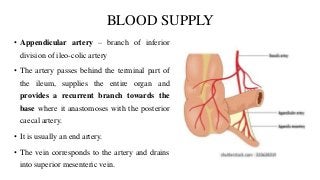
This document provides information about the large intestine, caecum, and appendix. It begins with an introduction to the large intestine and its differences from the small intestine. It then discusses the sub-divisions of the large intestine including the caecum, appendix, colon, and rectum. The document describes the characteristic features of the large intestine such as the taeniae coli, sacculations, and appendices epiploicae. It provides details on the caecum, appendix, their blood supply, relations, and clinical relevance. In summary, the document is an anatomical overview of the large intestine with a focus on the caecum and appendix.