1. The document summarizes the anatomy and blood supply of the stomach, small intestine, large intestine, and rectum.
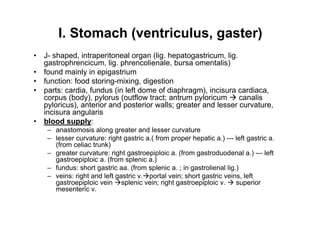
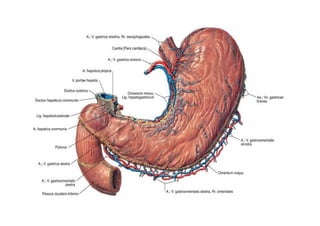
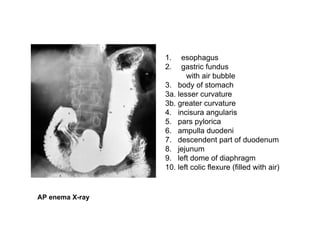
2. The stomach is J-shaped and located in the epigastrium. It receives blood supply from branches of the celiac trunk and superior mesenteric artery.
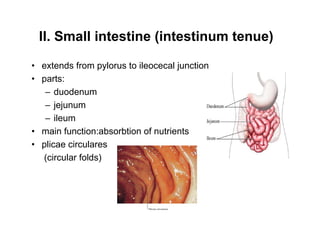
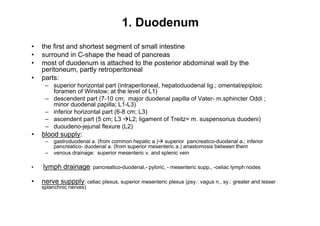
3. The small intestine extends from the pylorus to the ileocecal junction and consists of the duodenum, jejunum, and ileum. The duodenum receives its blood supply from the gastroduodenal artery while the jejunum and ileum receive branches from the superior mesenteric artery.
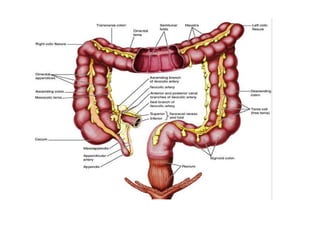
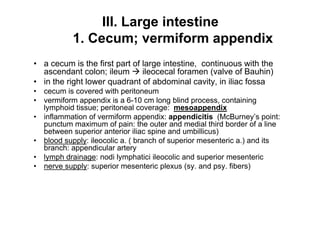
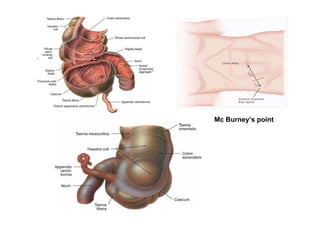
4. The large intestine consists of the cecum