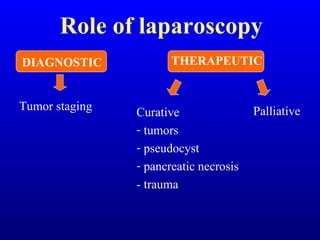
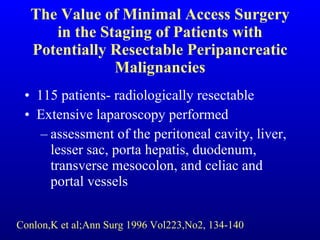
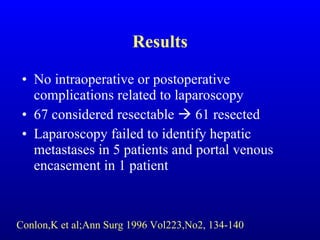
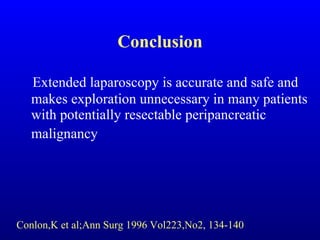
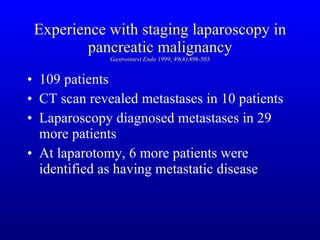
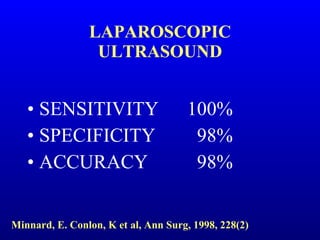
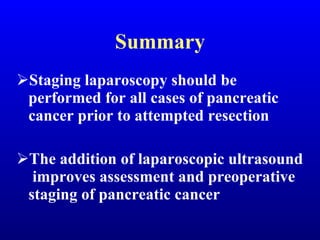
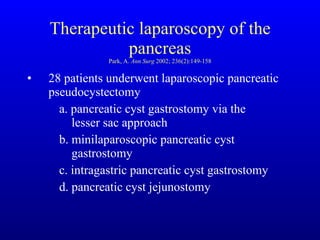
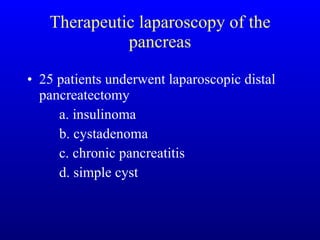
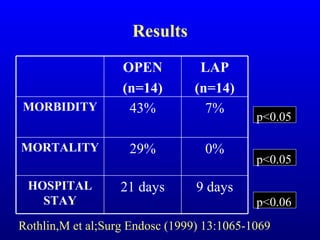
Laparoscopy and laparoscopic ultrasound improve staging of pancreatic cancer and help determine resectability, avoiding unnecessary surgery. Laparoscopic techniques can treat some benign and malignant pancreatic tumors, as well as pancreatic trauma, pseudocysts, and provide palliative bypass when cancer is unresectable, with benefits of less morbidity, mortality, and shorter hospital stays compared to open surgery.