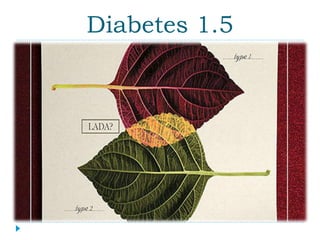
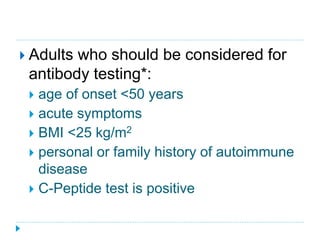
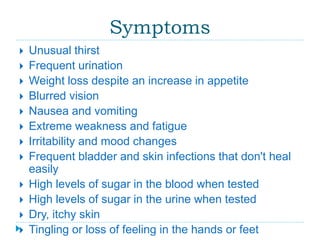
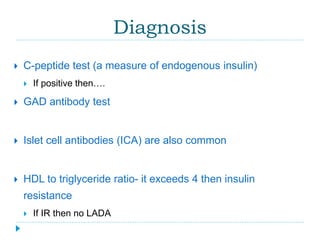
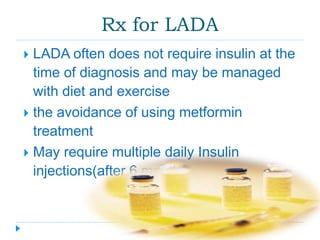
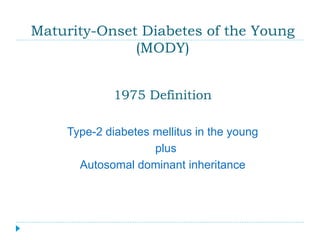
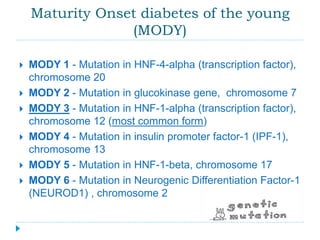
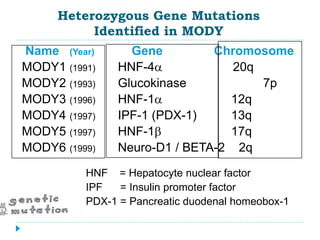
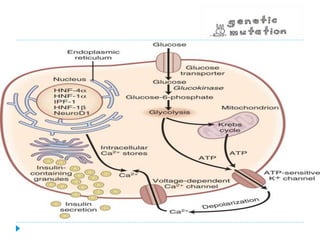
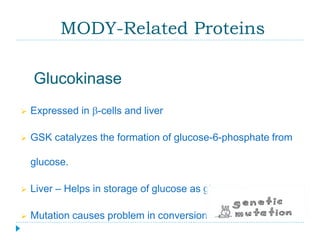
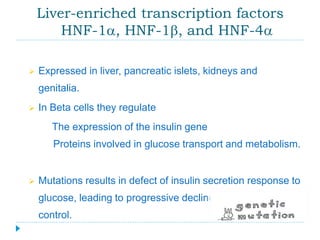
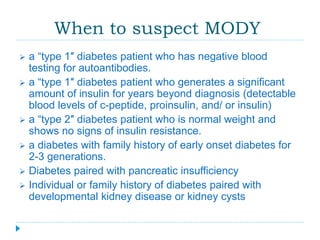
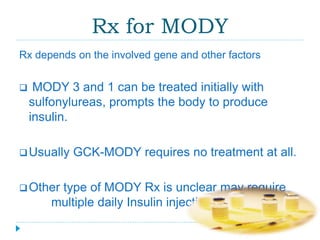
Latent autoimmune diabetes in adults (LADA) is often misdiagnosed as type 2 diabetes; it typically presents in individuals over 50 and progresses to insulin dependence within six years. Maturity-onset diabetes of the young (MODY) is characterized by genetic mutations affecting insulin secretion, resulting in early-onset type 2 diabetes and various treatment needs depending on the specific gene involved. Diagnosis for both conditions includes assessing symptoms, antibody testing, and C-peptide levels to differentiate from other diabetes types.