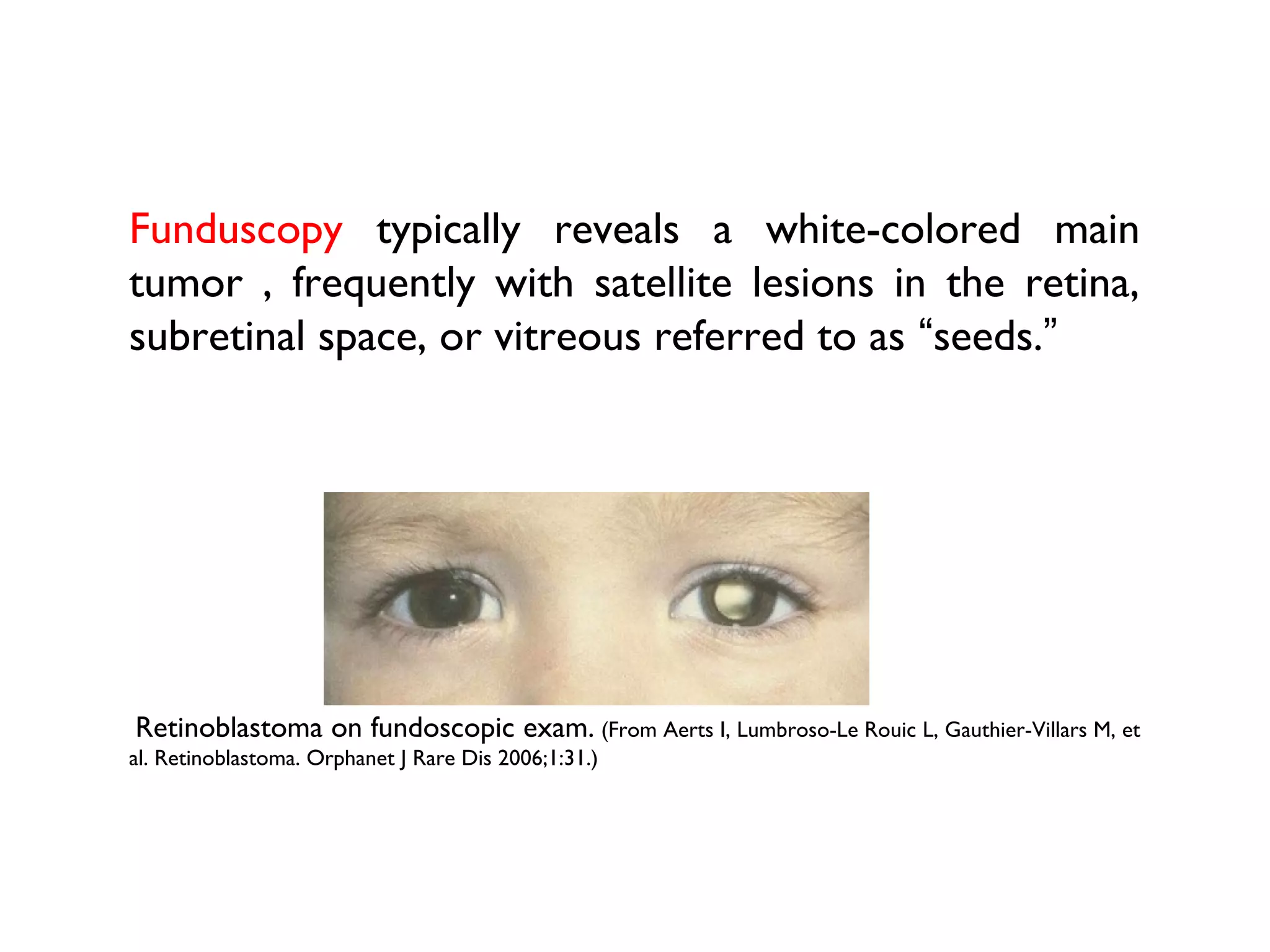
Retinoblastoma is a rare cancer that affects the retina in children. It is caused by mutations in the RB1 gene that regulates cell growth. The disease can be hereditary or sporadic. Presenting symptoms include leukocoria, strabismus, and vision loss. Diagnosis is usually made through eye examination and imaging tests like ultrasound and MRI. Treatment depends on disease stage and extent, and may include enucleation, chemotherapy, radiation therapy, cryotherapy, or brachytherapy to preserve vision and the eye. Retinoblastoma can spread from the eye to other parts of the body if not treated properly. Early detection and treatment are important for good outcomes.
























![Direct anterior field [Hungerford et al ]
Whole eye is treated
Disadvantage:
Cataract formation
Dose exits through brain
Lacrimal gland irradiation-
impaired tear production
Advantages:
Simple, easy to setup
Reproducible](https://image.slidesharecdn.com/retinoblastoma-160307140643/75/Retinoblastoma-29-2048.jpg)
![Anterior lens sparing technique [Abramson et al ]
Lateral D-shaped field: Day1-Day 4 by photons
Anterior electron beam field with central circular
contact lens as lens shaped shield: on Day 5
Unilateral disease:
one lateral field or
2 oblique portals
[superior and inferior]
Bilateral disease:
parallel opposed lateral fields](https://image.slidesharecdn.com/retinoblastoma-160307140643/75/Retinoblastoma-30-2048.jpg)















