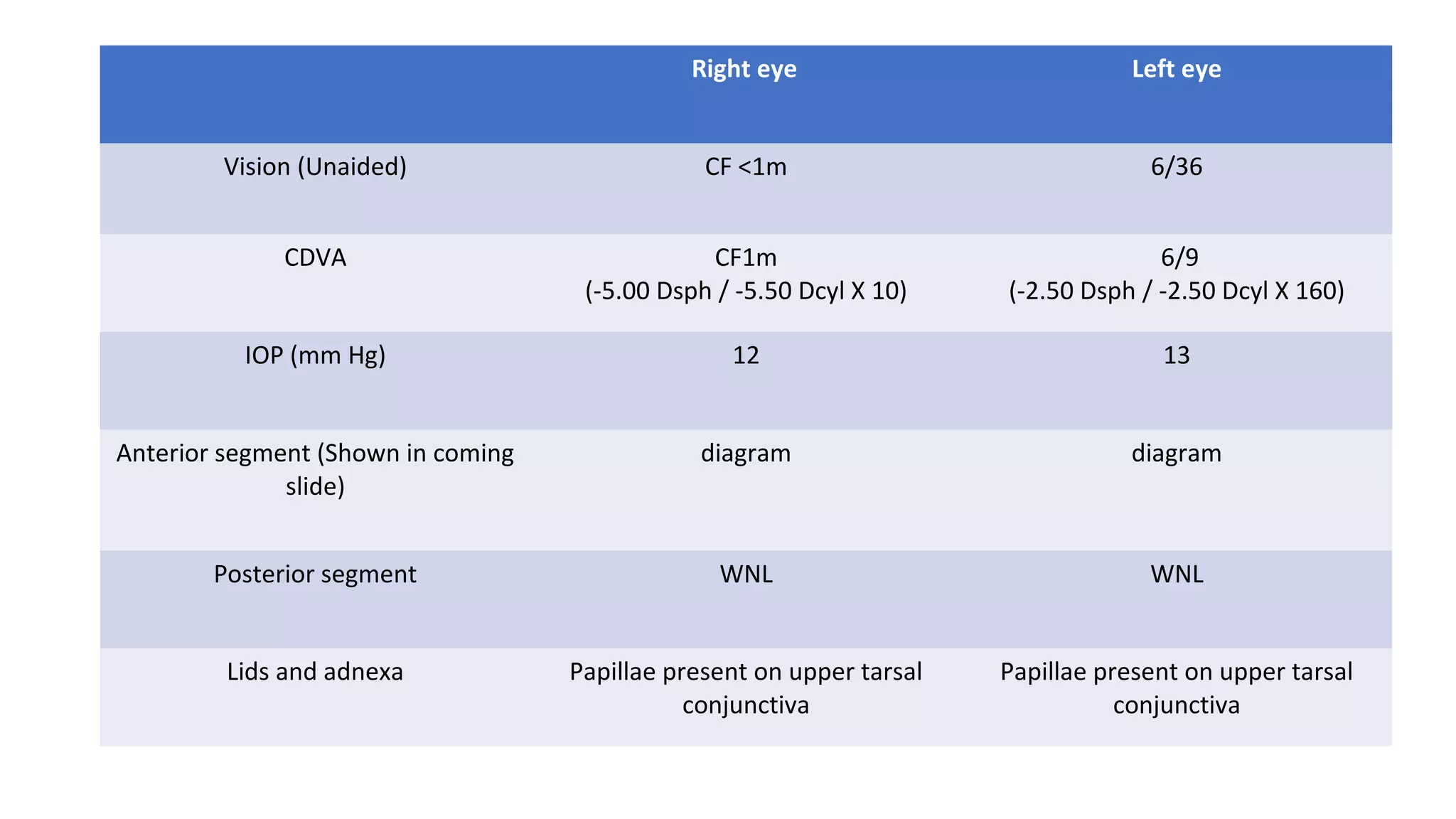
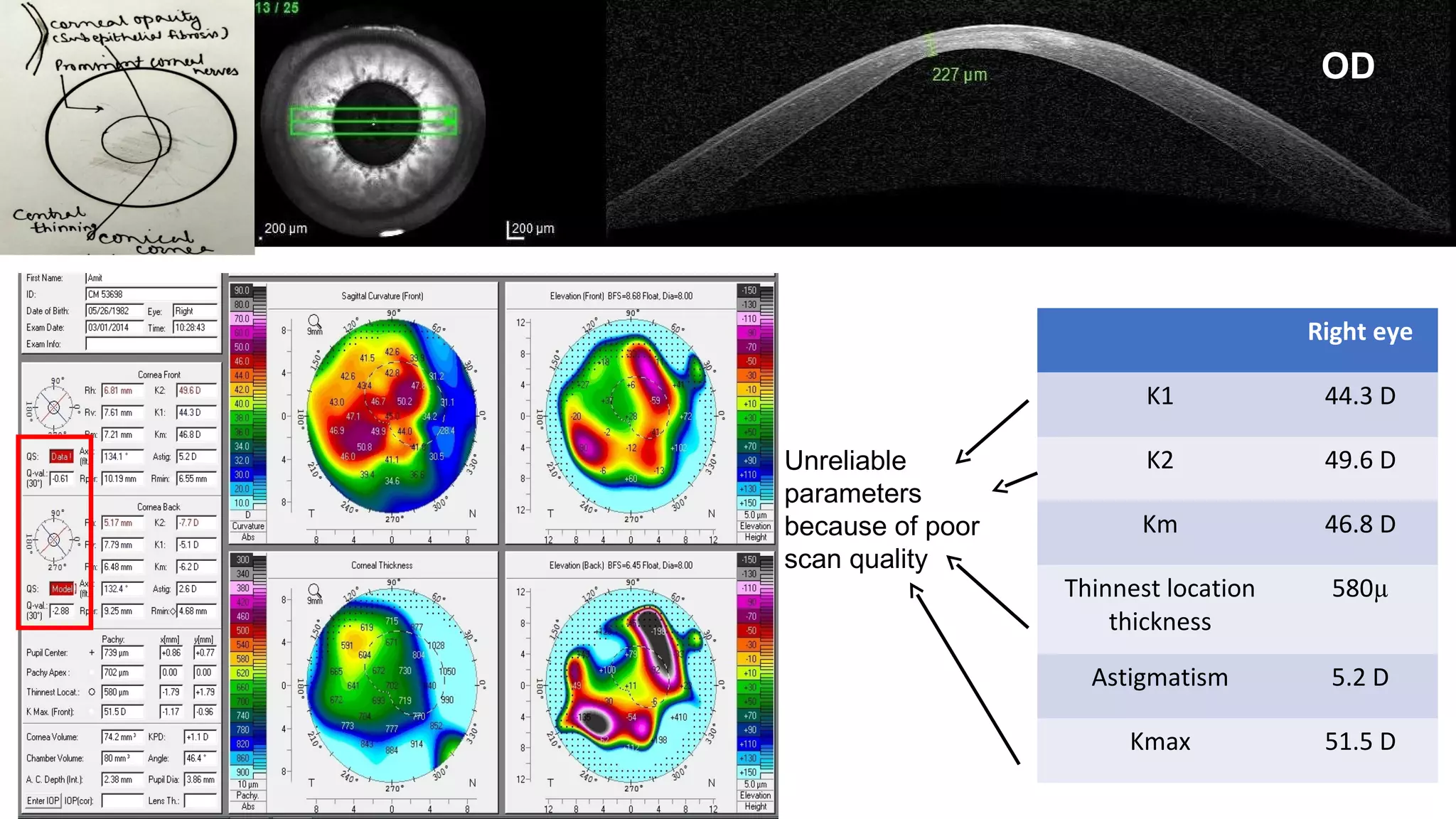
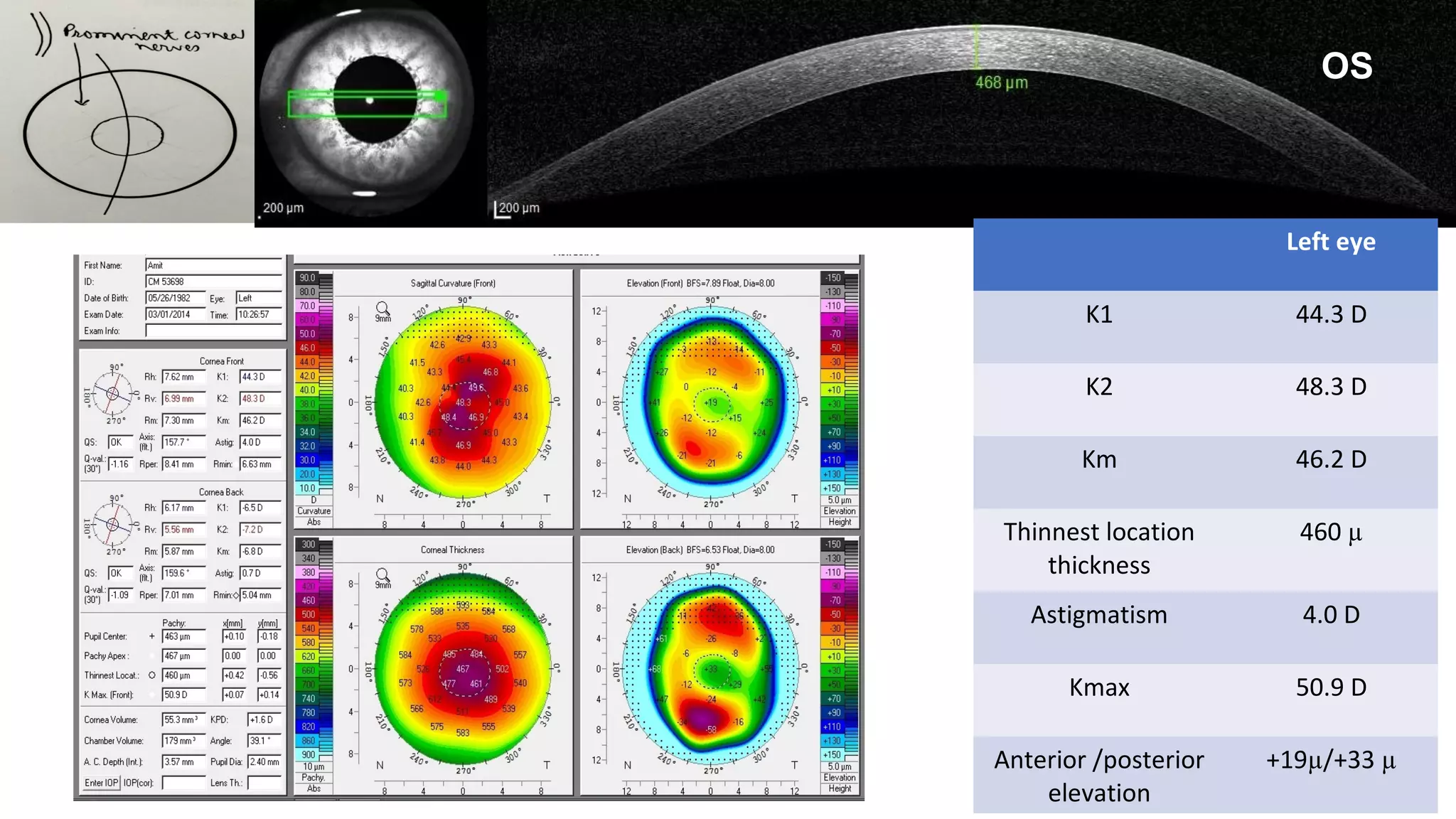
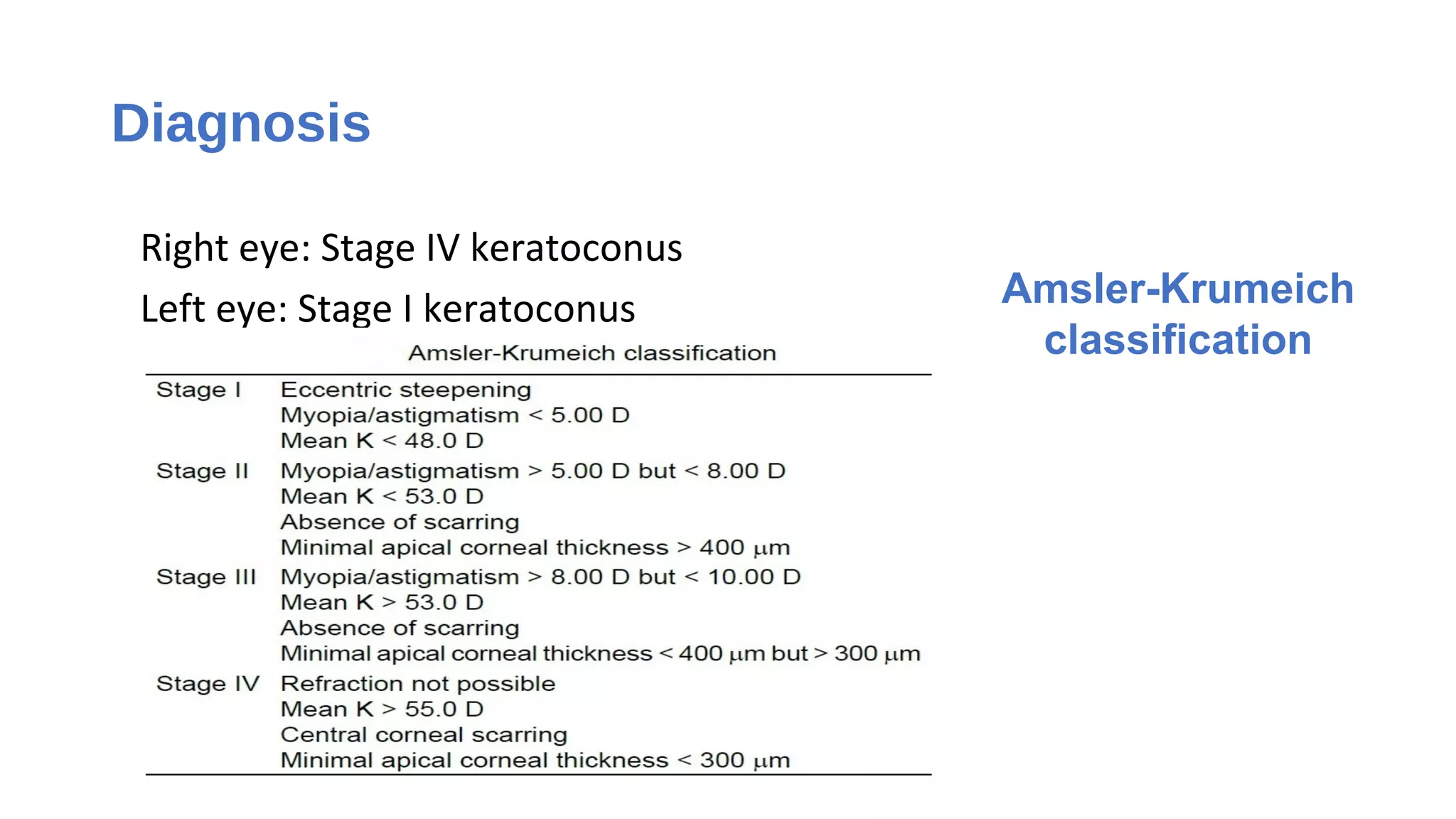
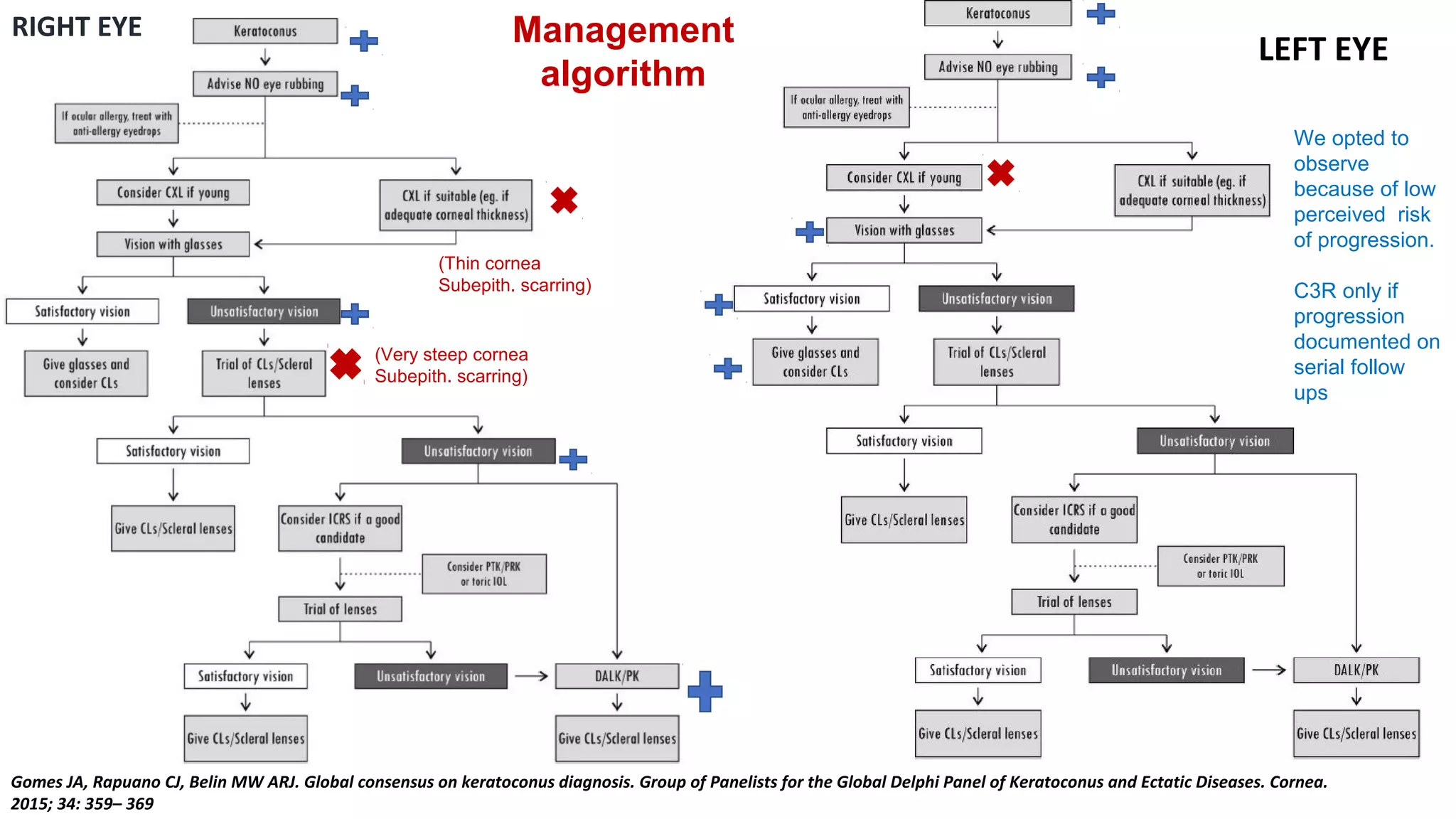
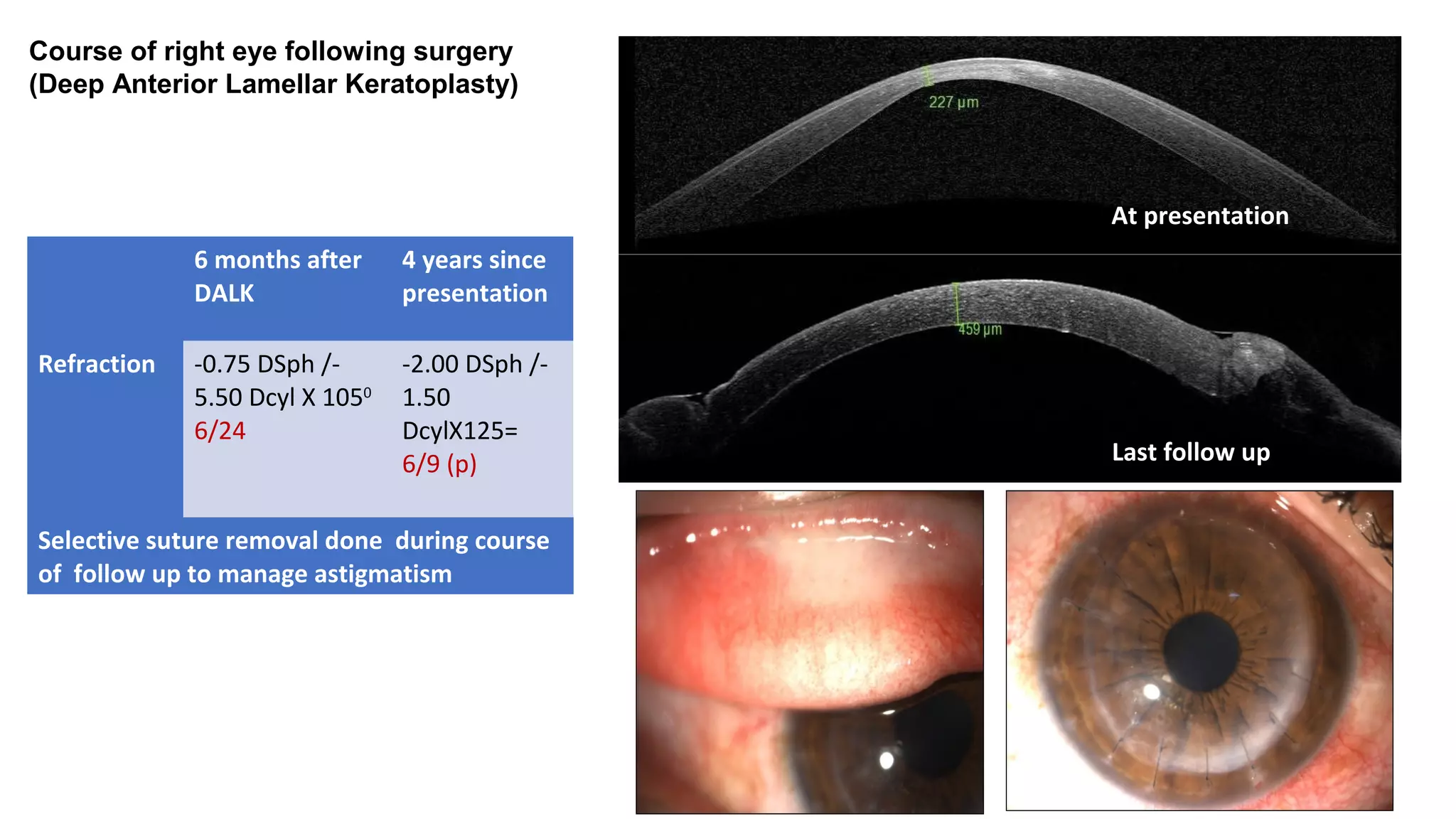
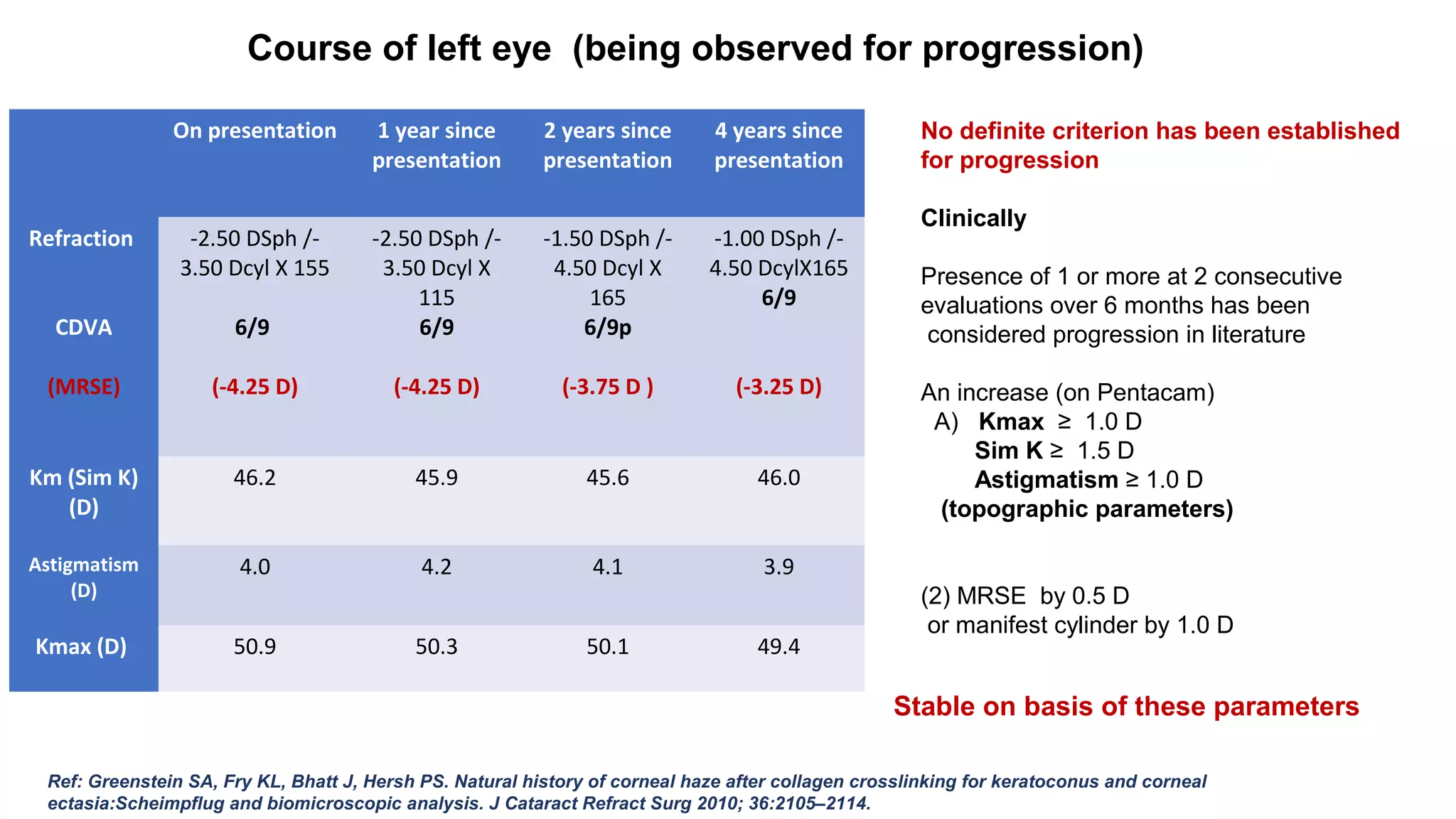
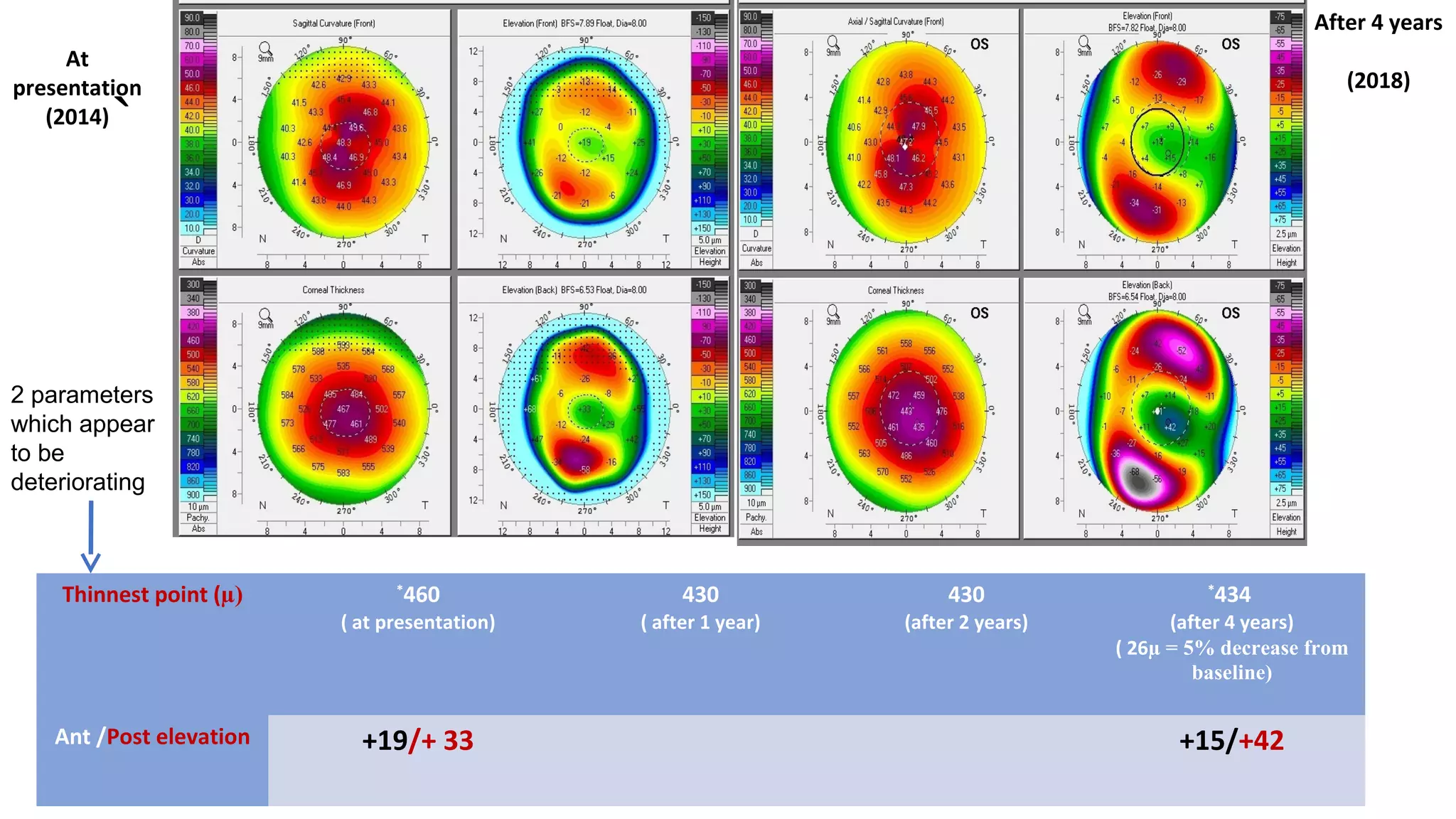
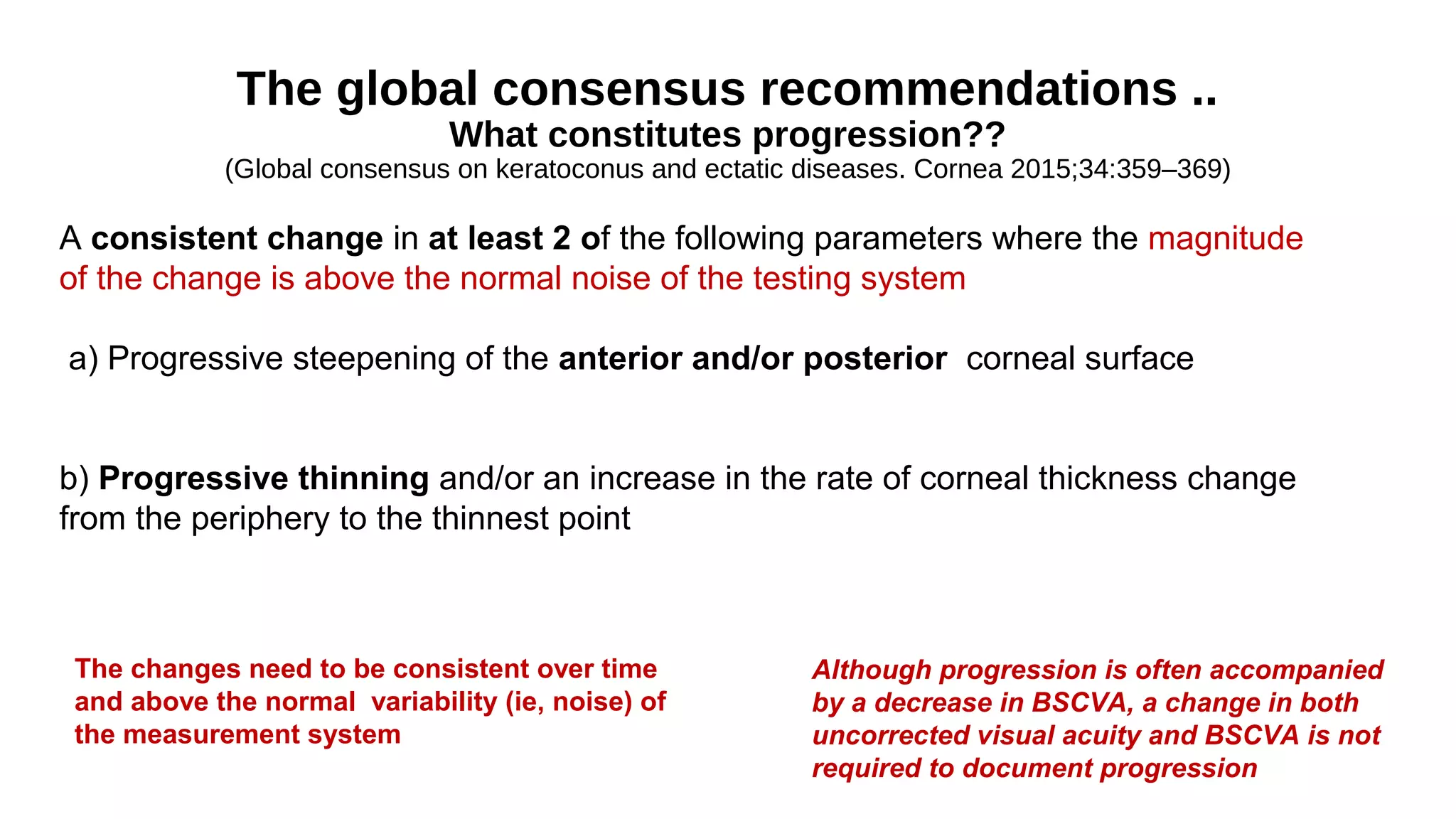
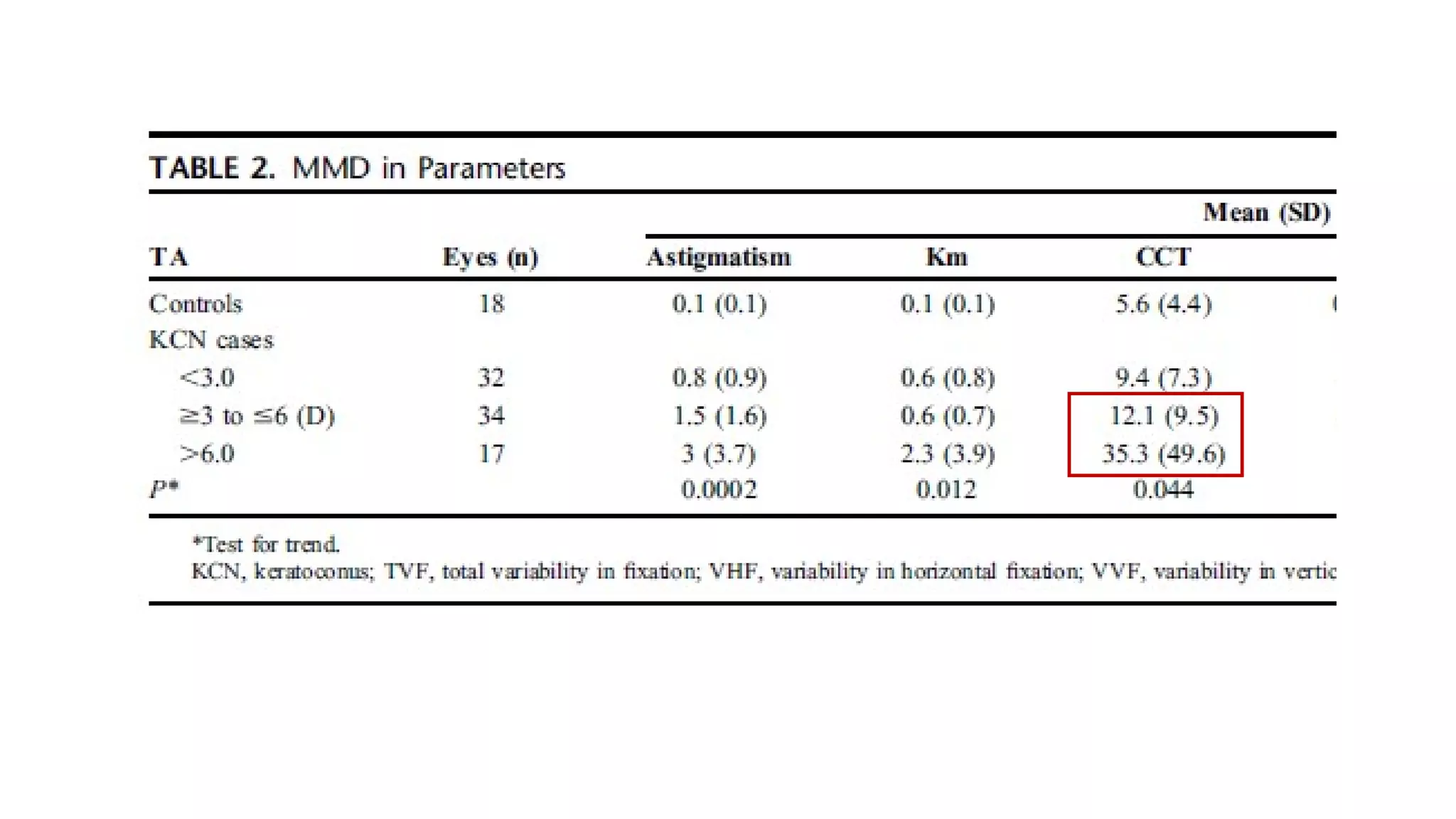
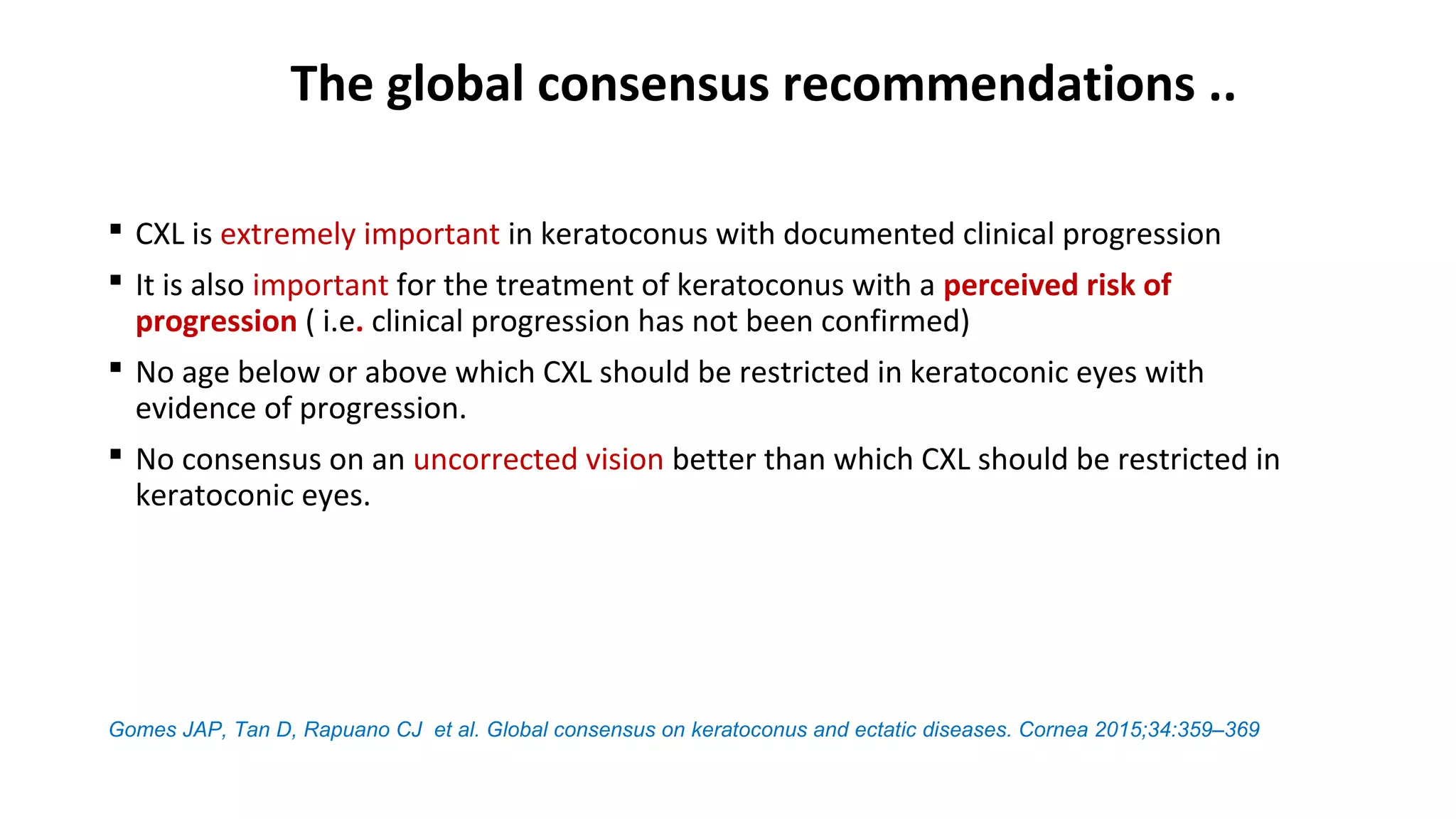
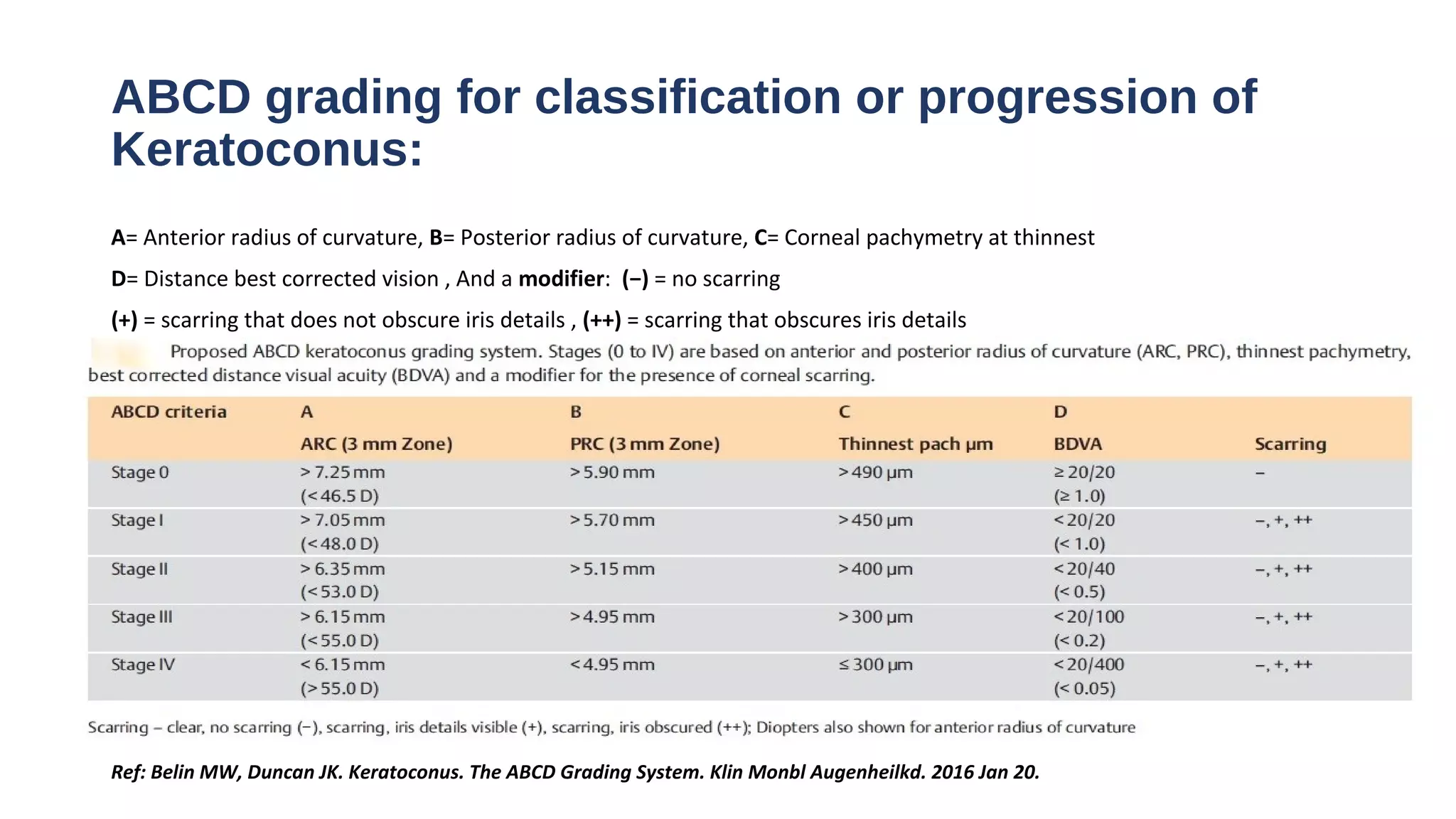
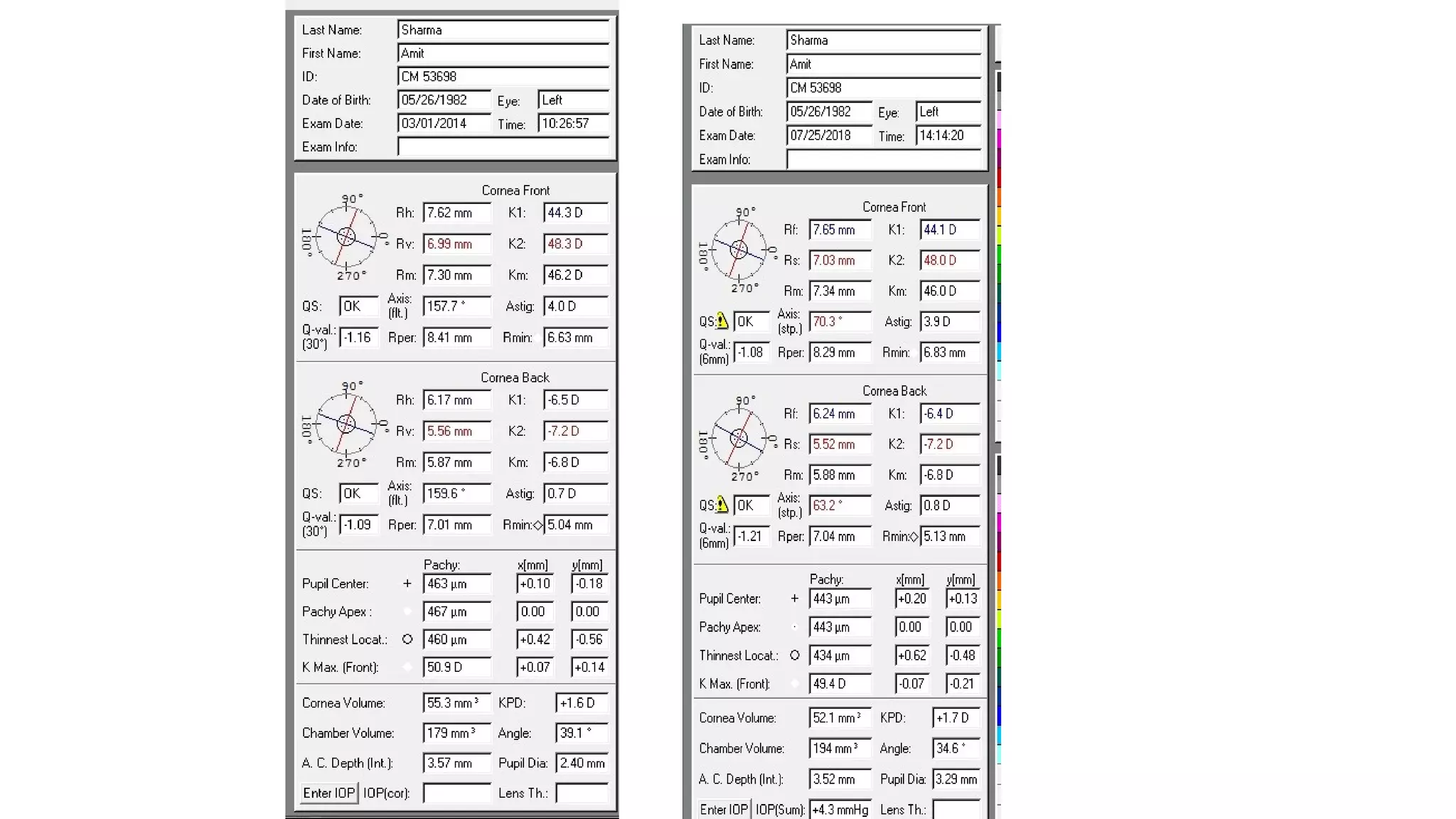
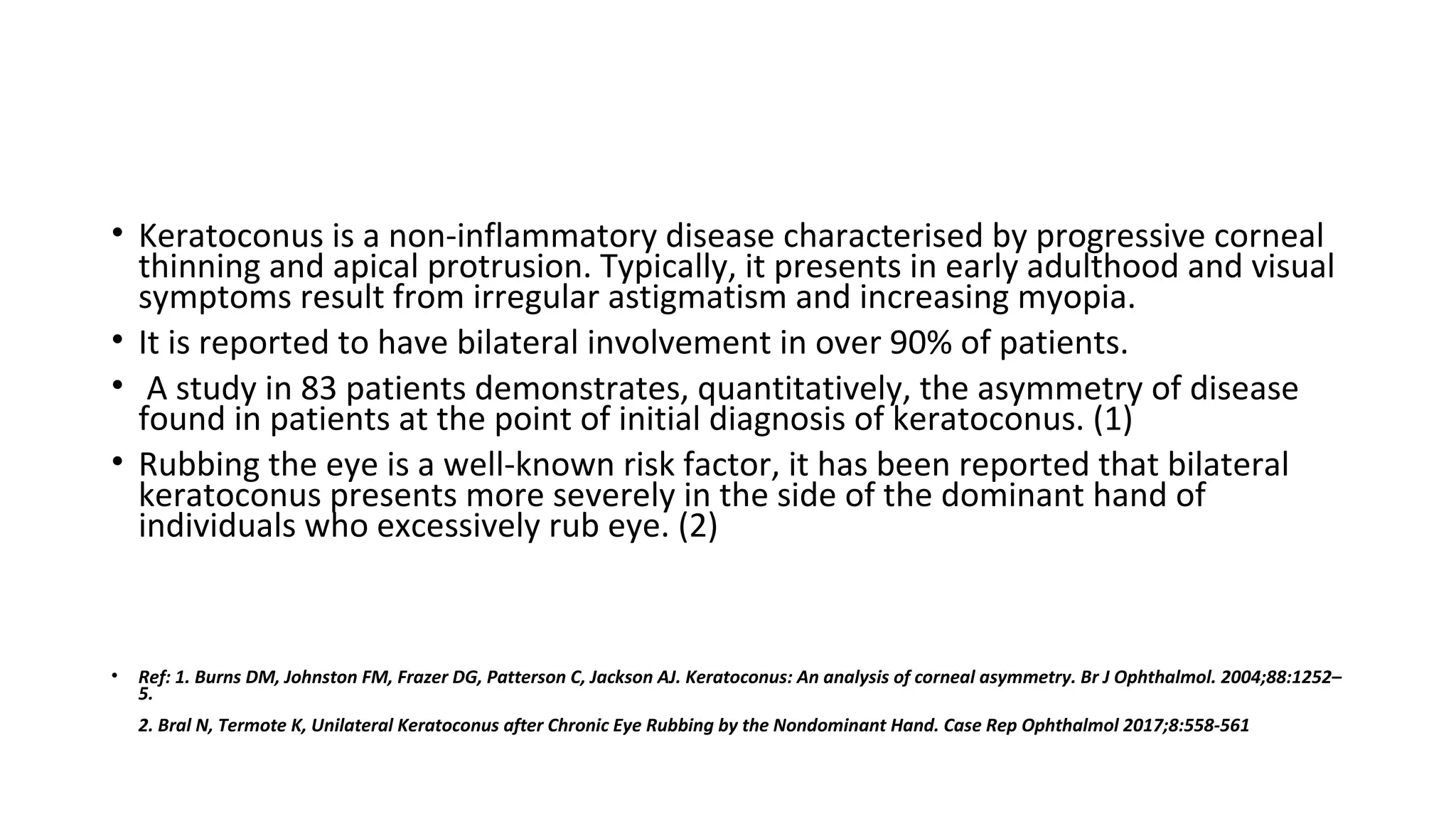
This document discusses the management of a 31-year-old male patient with bilateral asymmetric keratoconus that is more severe in the right eye. The right eye has stage IV keratoconus while the left eye has stage I. Deep anterior lamellar keratoplasty was performed on the right eye 4 years ago with good results. The left eye is being observed for progression. Parameters like corneal thickness, maximum keratometry, and anterior/posterior elevation have remained stable in the left eye over 4 years of follow-up based on global consensus recommendations for determining keratoconus progression. The limitations of the Amsler-Krumeich classification system for keratoconus are also discussed.