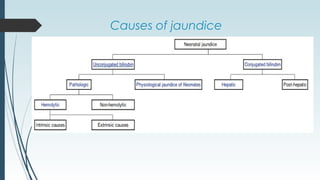
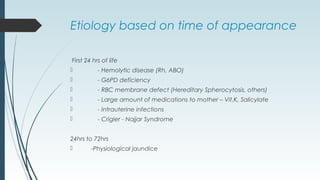
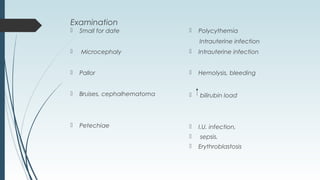
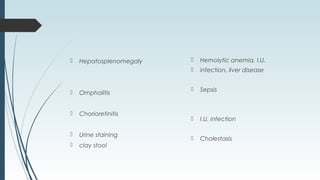
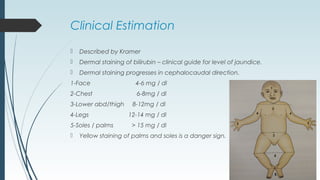
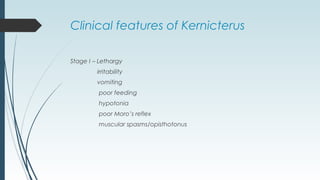
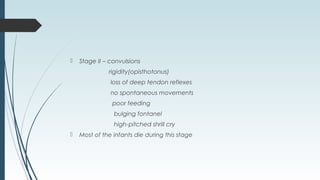
Neonatal jaundice is a yellowish discoloration of the skin due to high bilirubin levels in newborns. Nearly 60% of term newborns experience jaundice in the first week of life. High bilirubin levels can be toxic to the developing brain. Jaundice is caused by physiological or pathological factors like blood incompatibilities or liver diseases. It is important to monitor bilirubin levels closely in newborns as severe jaundice can lead to kernicterus, a neurological condition causing cerebral palsy or hearing loss.