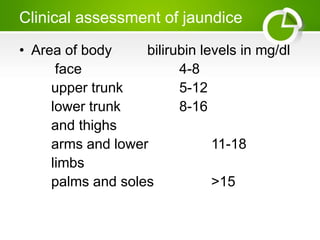
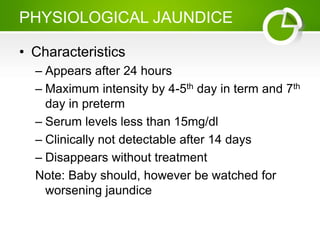
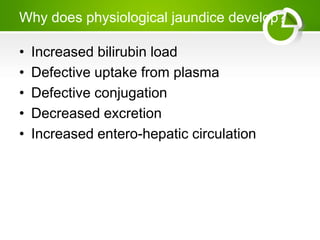
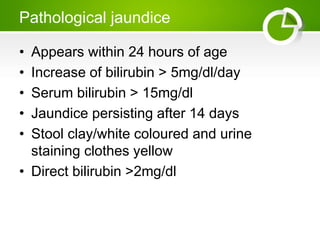
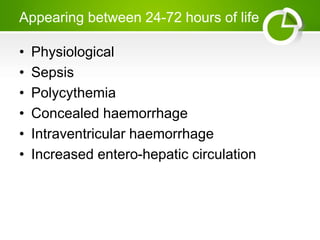
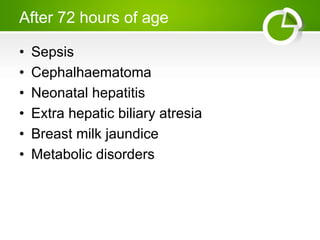
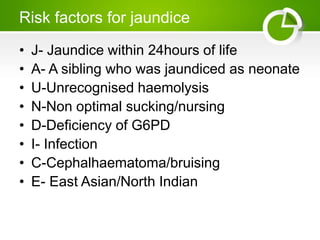
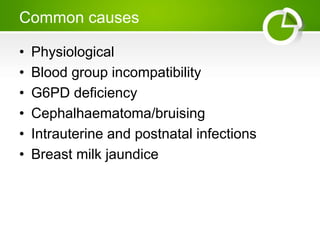
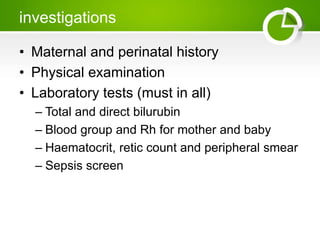
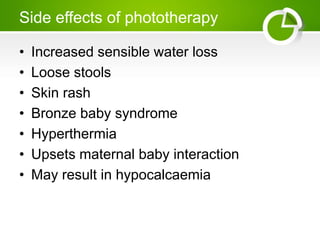
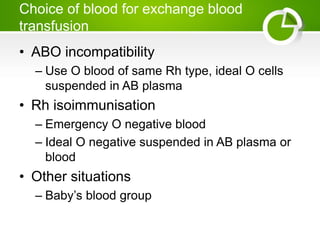
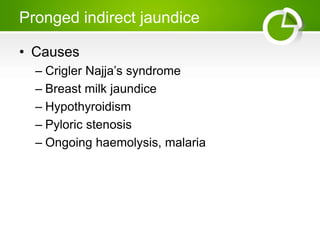
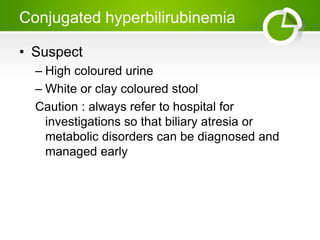
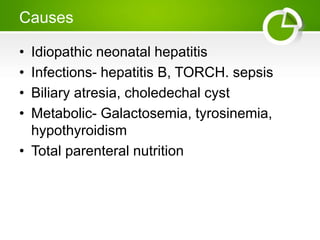
This document defines neonatal jaundice and outlines its causes and management. Physiological jaundice occurs in 60% of term and 80% of preterm babies and is caused by an imbalance between bilirubin production and excretion. Pathological jaundice appears within 24 hours and is investigated and treated. Management includes phototherapy to reduce bilirubin levels or exchange transfusion for severe cases. The document discusses evaluating jaundiced babies and monitoring bilirubin levels, feeding, and hydration.