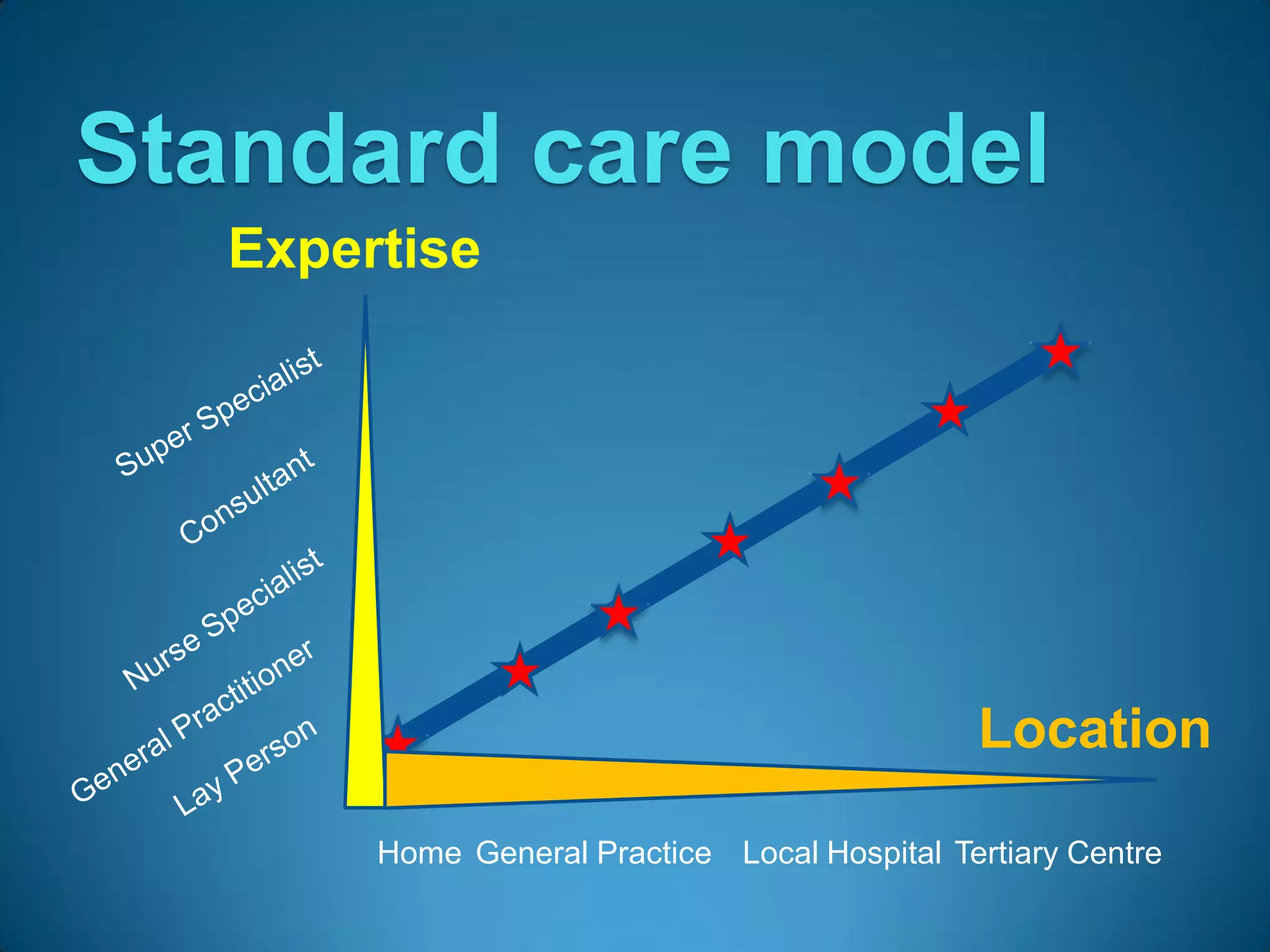
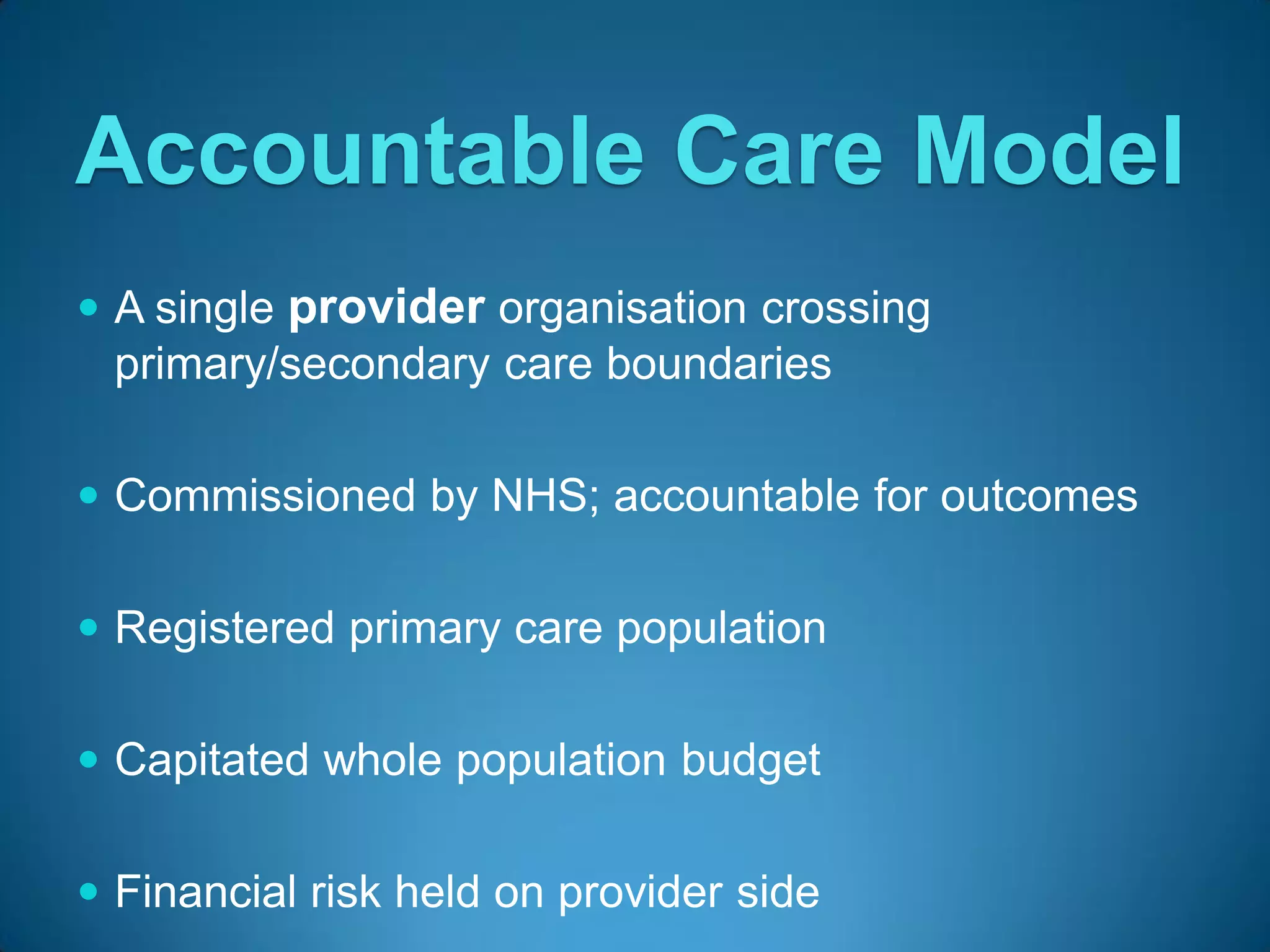
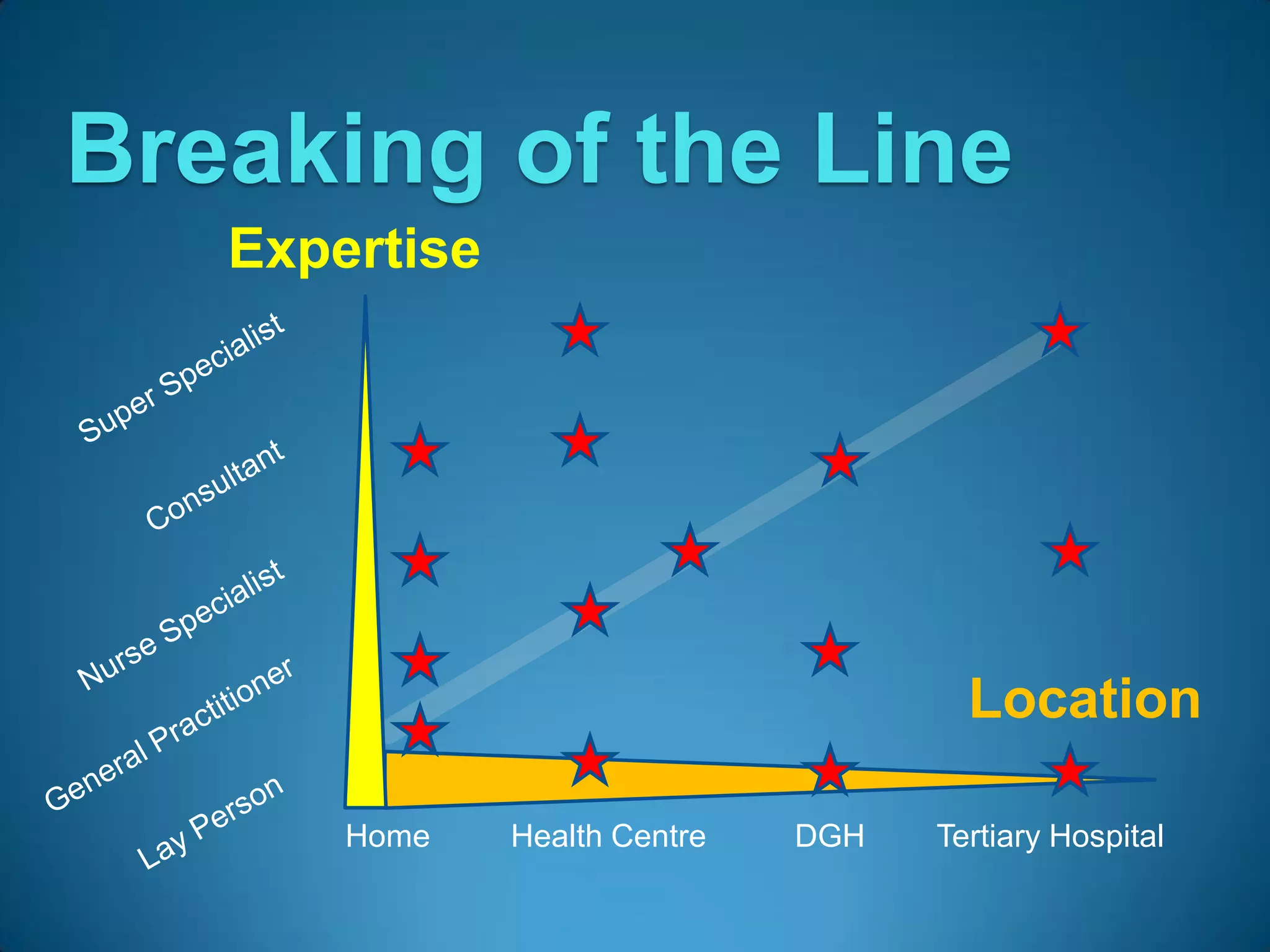
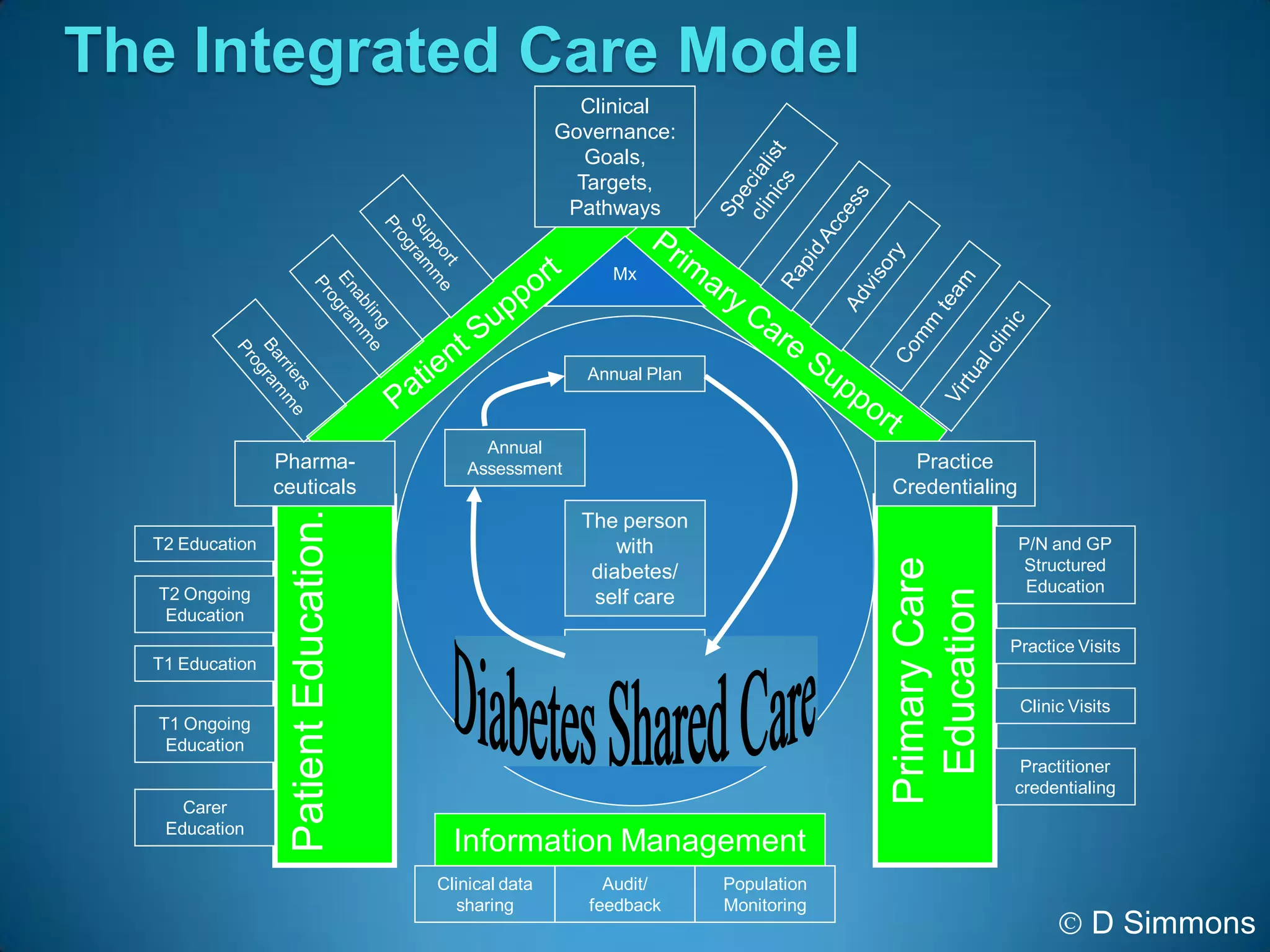
This document outlines the concept of an Accountable Care Organisation (ACO) proposed for Cambridge, England. The ACO would be a partnership between primary and secondary care providers to deliver care within a fixed budget. It would integrate services across home, community centers, and hospitals using a shared electronic patient record. The ACO aims to improve outcomes while reducing costs through clinical and financial integration. It would take on financial risk for the population it serves and be accountable to the NHS for outcomes. The document discusses potential advantages, priorities, and structure of the proposed ACO.