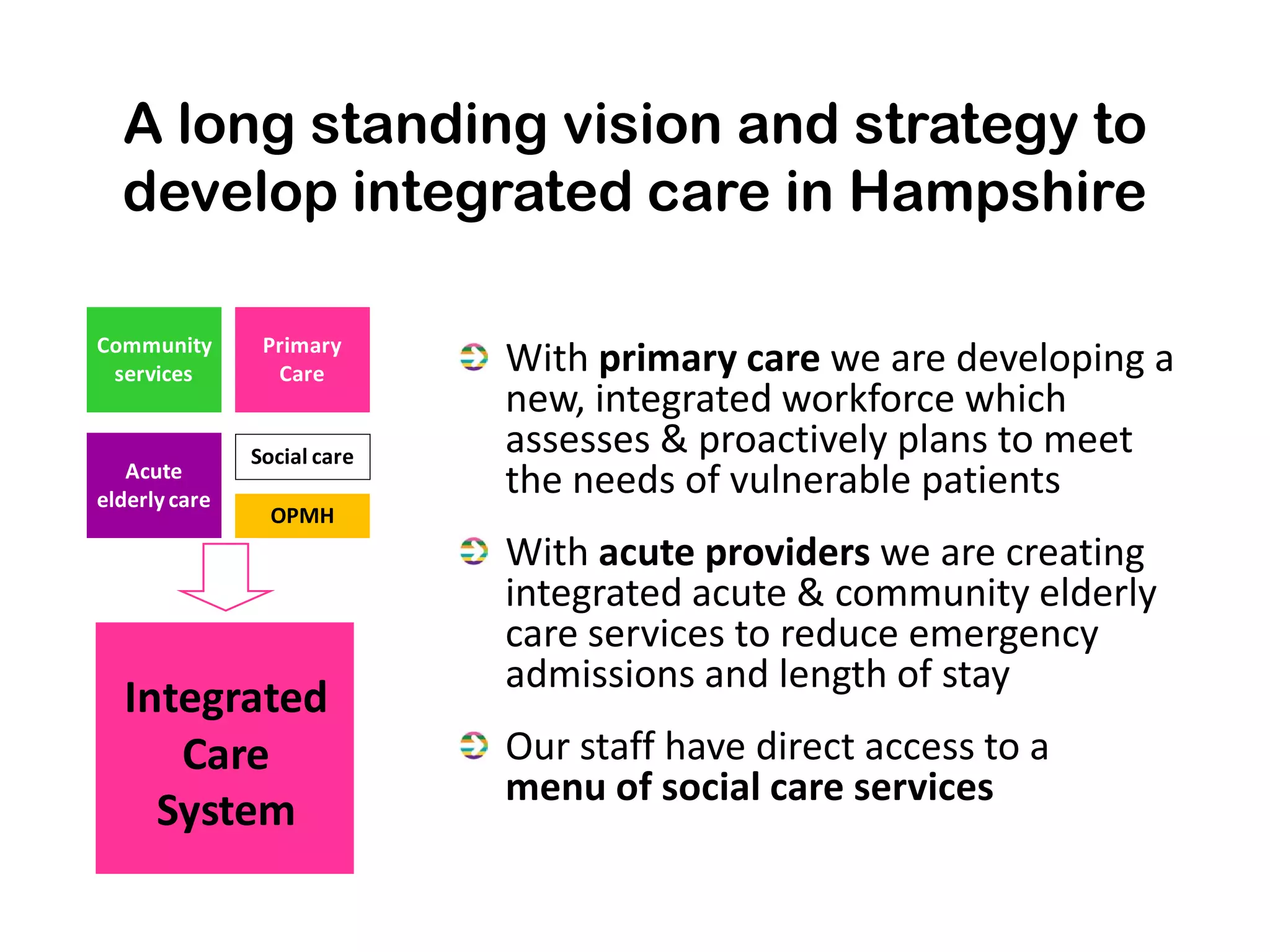
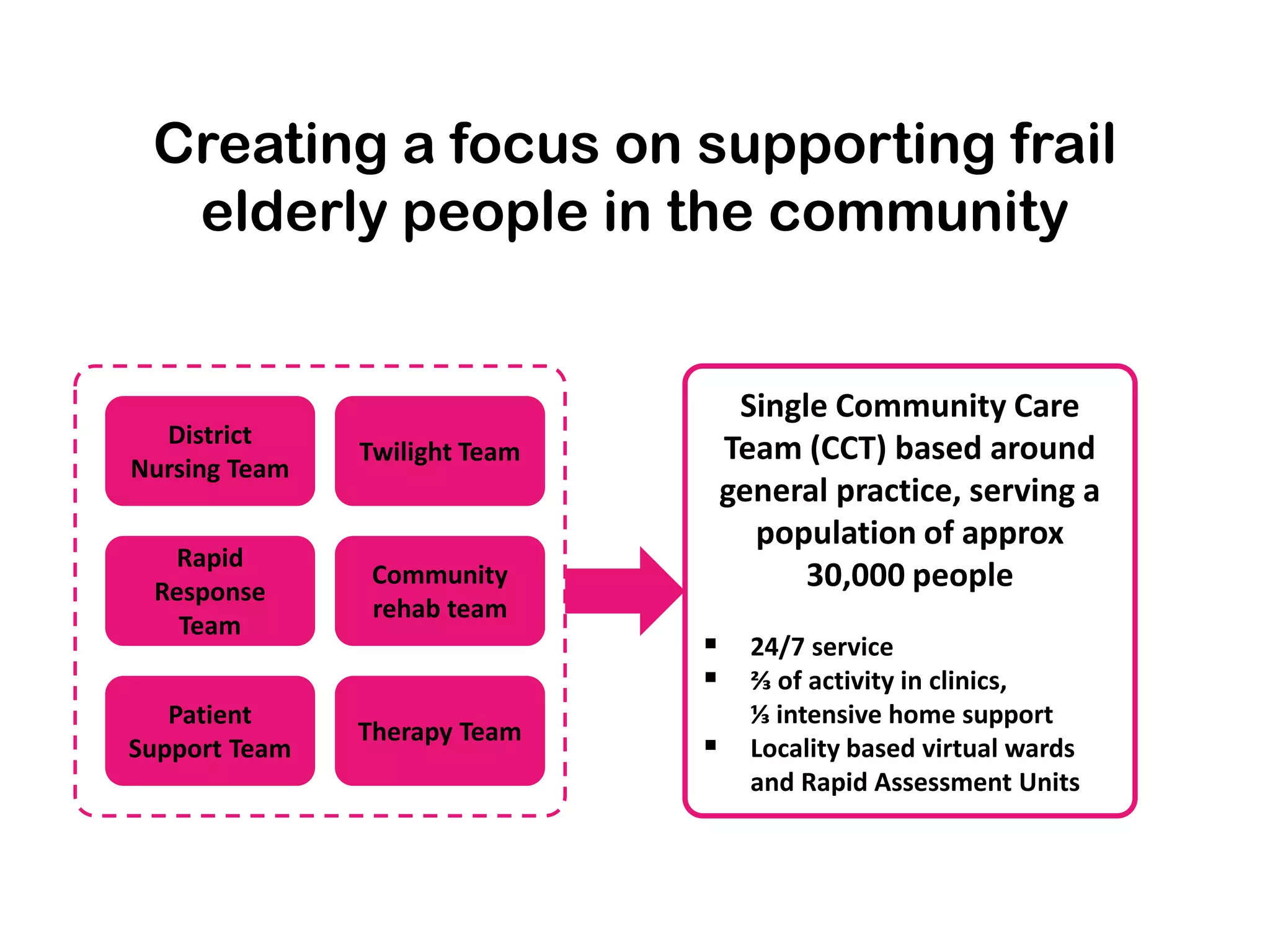
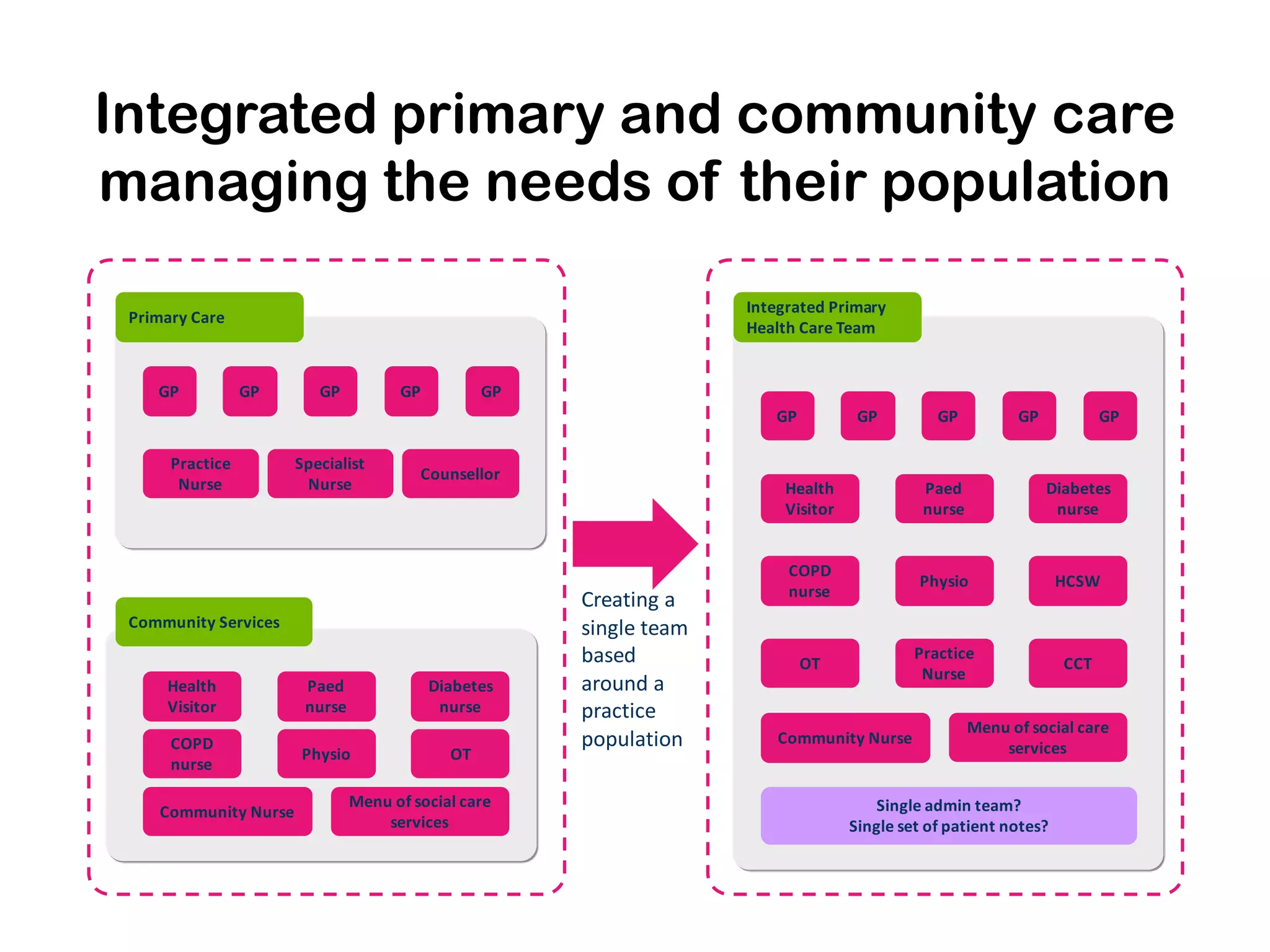
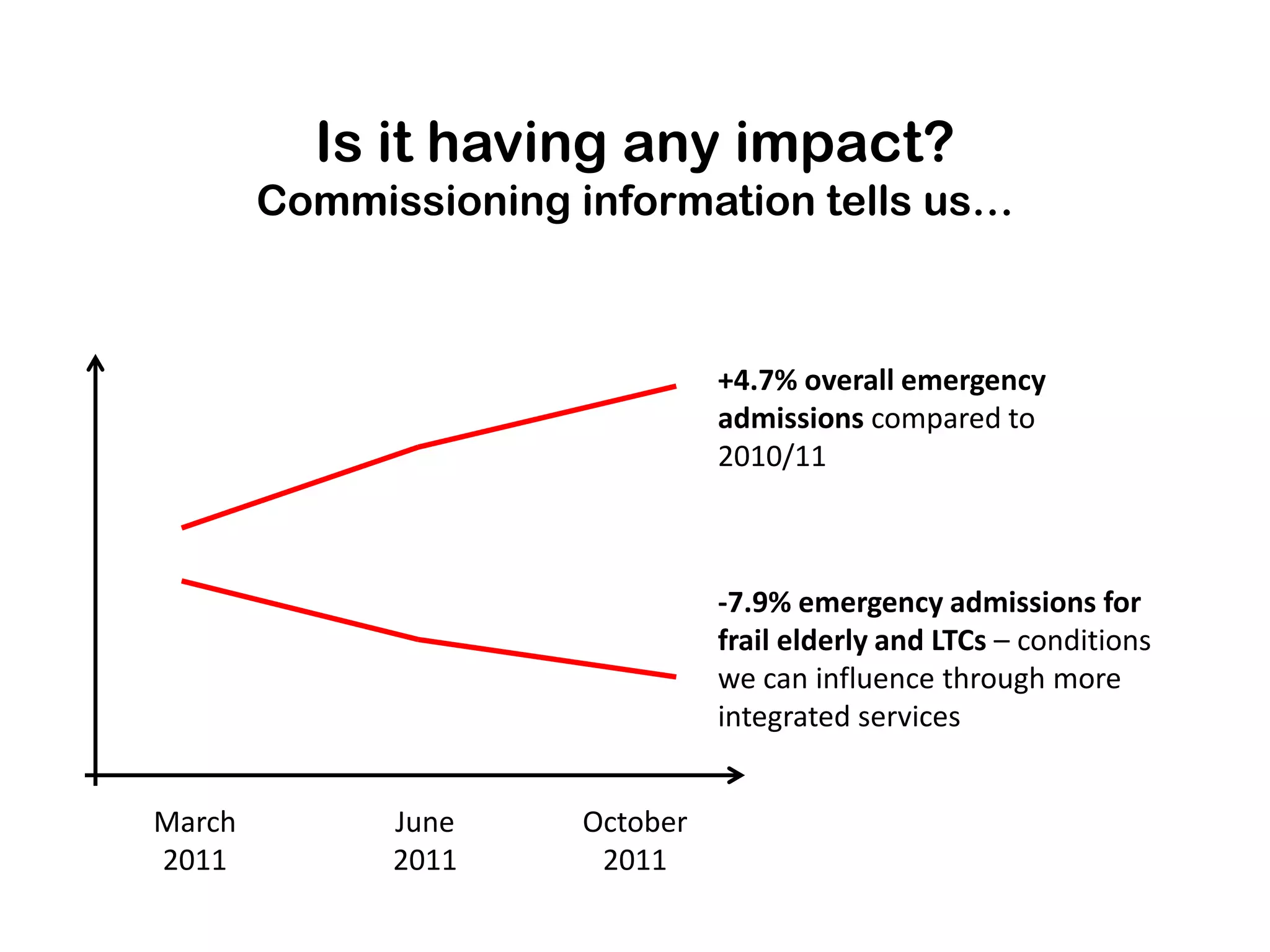
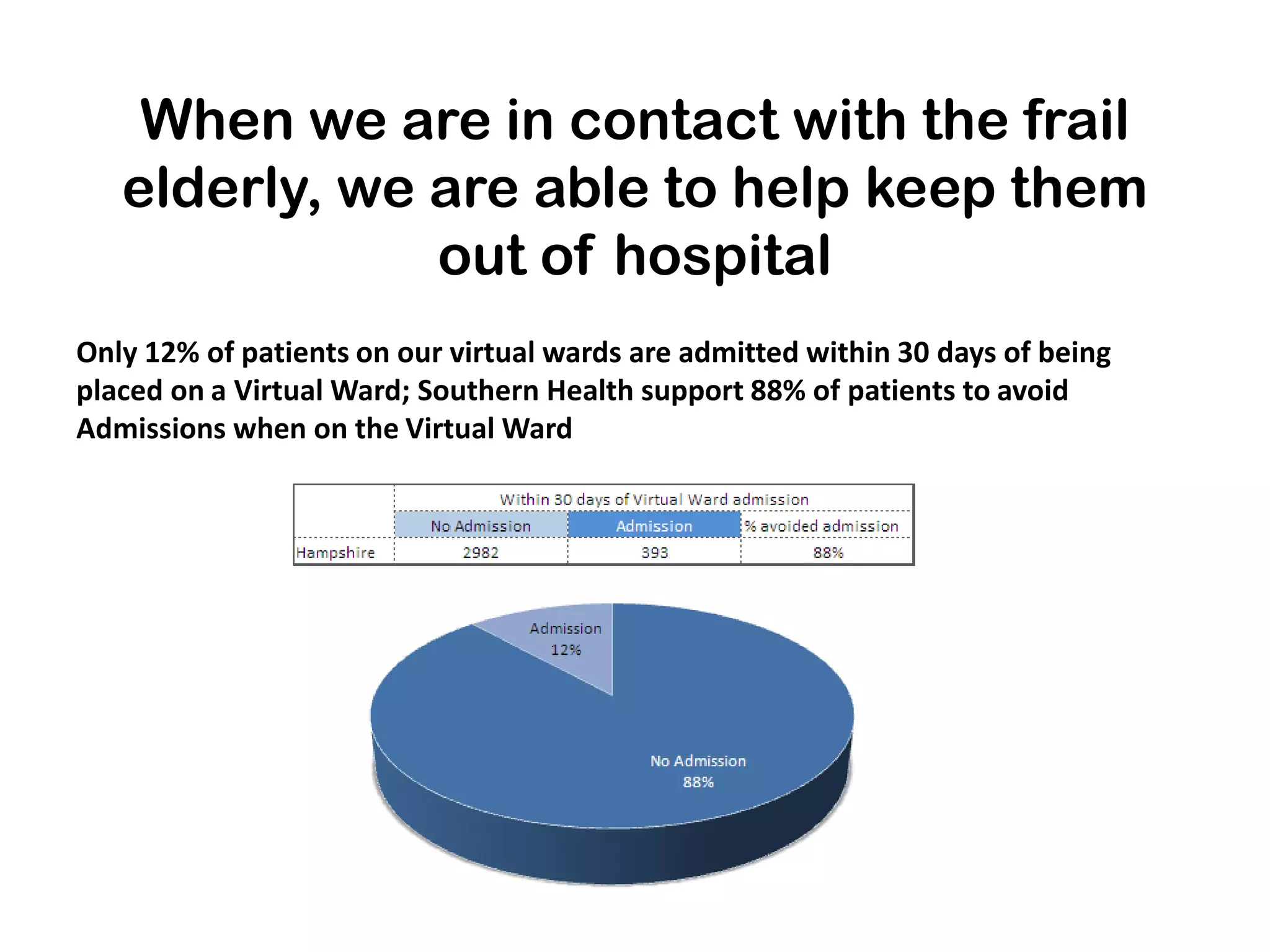
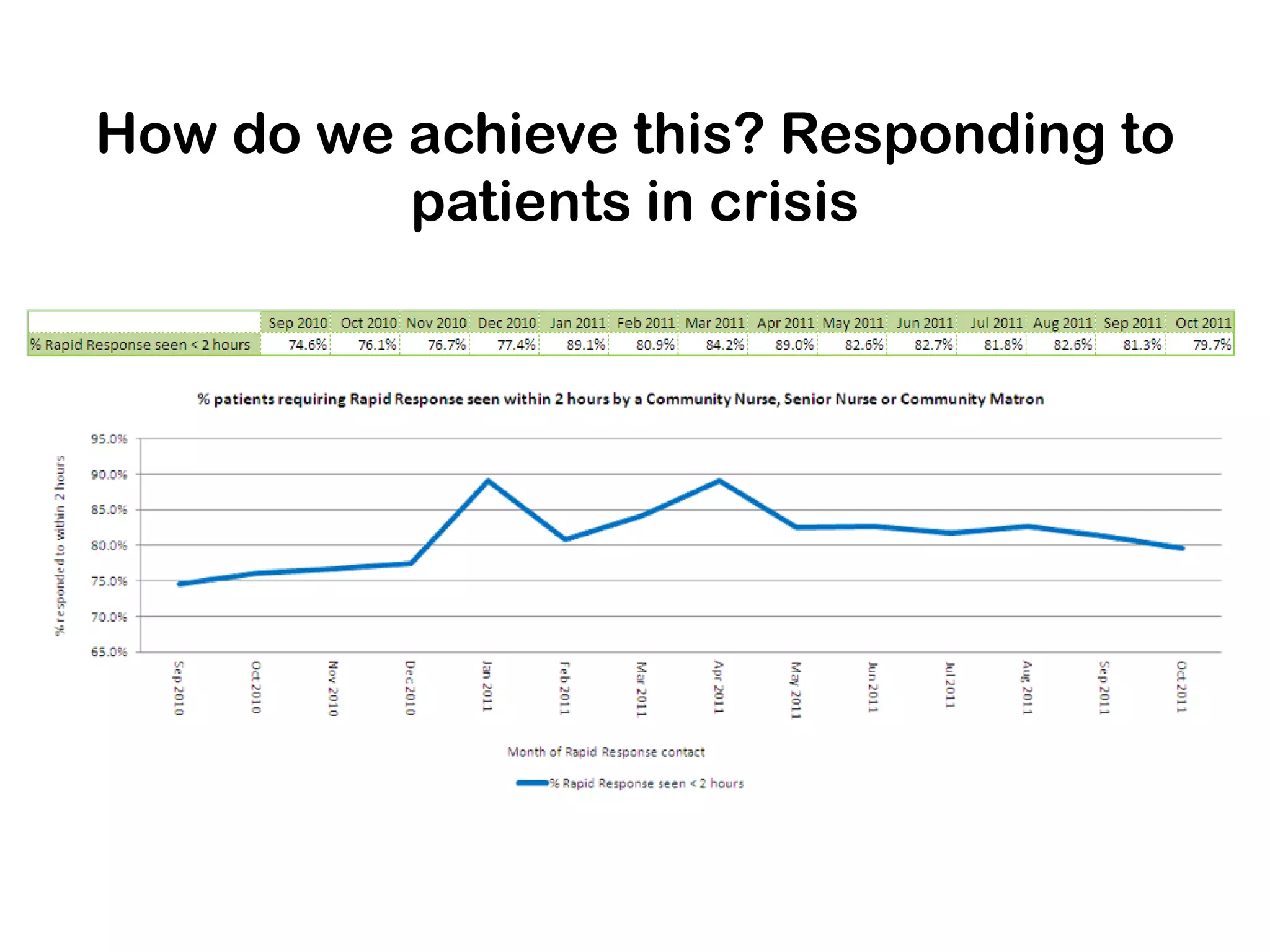
The document outlines Hampshire's initiative to develop an integrated care system aimed at improving community and mental health services by merging various service providers to enhance patient care. Key strategies include the formation of integrated teams and services, a focus on elderly care, and a commitment to redesigning healthcare delivery to reduce costs and improve outcomes. Data suggests that these changes are positively impacting emergency admissions, particularly for frail elderly patients, by enabling better support and care in the community.