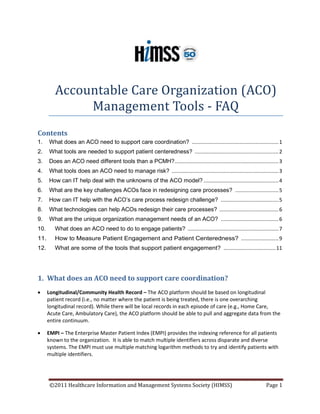
Accountable Care Organization (ACO) Management Tools - FAQ
- 1. Accountable Care Organization (ACO) Management Tools - FAQ Contents 1. What does an ACO need to support care coordination? ............................................................ 1 2. What tools are needed to support patient centeredness? .......................................................... 2 3. Does an ACO need different tools than a PCMH? ........................................................................ 3 4. What tools does an ACO need to manage risk? .......................................................................... 3 5. How can IT help deal with the unknowns of the ACO model? .................................................... 4 6. What are the key challenges ACOs face in redesigning care processes? .............................. 5 7. How can IT help with the ACO’s care process redesign challenge? ........................................ 5 8. What technologies can help ACOs redesign their care processes? ......................................... 6 9. What are the unique organization management needs of an ACO? ........................................ 6 10. What does an ACO need to do to engage patients? ............................................................... 7 11. How to Measure Patient Engagement and Patient Centeredness? .......................... 9 12. What are some of the tools that support patient engagement? .................................... 11 1. What does an ACO need to support care coordination? • Longitudinal/Community Health Record – The ACO platform should be based on longitudinal patient record (i.e., no matter where the patient is being treated, there is one overarching longitudinal record). While there will be local records in each episode of care (e.g., Home Care, Acute Care, Ambulatory Care), the ACO platform should be able to pull and aggregate data from the entire continuum. • EMPI – The Enterprise Master Patient Index (EMPI) provides the indexing reference for all patients known to the organization. It is able to match multiple identifiers across disparate and diverse systems. The EMPI must use multiple matching logarithm methods to try and identify patients with multiple identifiers. ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 1
- 2. • Health Information Exchange (HIE) - The HIE allows multiple care providers and stakeholders in a community to share patient data in a secure, confidential manner. Data from multiple sources is collected and exchanged based on interoperability standards. The HIE should include a semantic mapping framework that enables discrete data elements to be harvested and presented in custom displays for clinical review at the point of care, for analytics and to meet the requirements of meaningful use. • Hierarchical Data Security - The system should allow for a multi-layered, configurable role-based security model to ensure compliance with privacy and confidentiality regulations. Access to patient records can be based on a region, organization, clinical care team, provider, etc., using role-based access. All data exchanged is in encrypted form. Every field in the database can be audited. In addition the platform should include break-glass functionality to get temporary emergency access to data such as mental health or communicable disease data. • Collaborative Clinical Decision Support – This is the ability to access the data collected in the Health Information Exchange with added chronic disease management tools to be able to provide community-based information to providers as they deliver care. For example, in the case of a diabetic patient, at the point of the care, the virtual care team, including the PCP, endocrinologist, dietician, physical therapist, and patient all have access to up-to-date information, including the last blood sugar reading and the HbA1C level. In addition, the provider has data on the specific care plan to be followed for this patient. • Provider-to-Provider Communication Tools - Examples of this include secure provider-to-provider email as well as an ability to send out clinical alerts. The clinical alerts would inform a specific caregiver or team of caregivers about an elevated lab result, a change to a patient’s medication, a recent MRI report, etc., in a secure fashion. • Integrated Workflow Management – As part of the platform and its team-based approach and Collaborative Clinical Network Management functionality, all members of the care team can be following a care plan for a given patient in which all members of the care team have access to all information on that patient in a secure fashion with role-based access. • Active Care Management - Active care management utilizes (evidence-based) care protocols or pathways to notify all the participants involved in care delivery, including the patient, of their roles and responsibilities and required interventions. On-going assessment and analysis of service interventions, clinical and disease markers enable automated feedback to modify specific care delivery tasks, and recommend changes to improve care protocols or pathways. 2. What tools are needed to support patient centeredness? The ACO Platform should be based on a longitudinal patient record model (i.e. no matter where the patient is being treated, there is one overarching longitudinal record). While there will be local records in each episode of care (e.g., Home Care, Acute Care, Ambulatory Care), the ACO platform should be able to pull and aggregate data from the entire community. The ACO platform should enable all stakeholders, including patients, to get consistent and comprehensive information about their care. ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 2
- 3. 3. Does an ACO need different tools than a PCMH? Patient Centered Medical Homes and ACOs are not competitive. They are complementary. PCMH can operate within an ACO structure. In this context, most tools needed by a PCMH will also be useful for an ACO. In some cases, ACOs will need additional functionality from the same tools. In other cases, ACOs will need additional tools. The table below summarizes the different tools and their use between these two models: Tool PCMH ACO Electronic health record (EHR) Primary practice EHR may be Longitudinal/community is sufficient if data from care highly recommended, including team can be integrated enterprise master patient index (EMPI) Health information exchange Preferred but not necessary May be necessary to populate longitudinal EHR Clinical decision support Tools integrated with practice Must be collaborative and EHR may be sufficient shared across the organization Care management Passive data sharing may be Active tools are highly sufficient preferable Quality reporting Provider-centric Population-centric Clinical analytics Support continuous quality Support continuous quality and improvement outcomes improvement, including patient and financial outcomes Organization management Practice management ACO budgeting/cost accounting; ACO legal/contract management; Operational management with hierarchical security and functionality 4. What tools does an ACO need to manage risk? At their core, ACOs are a means for transferring certain risks associated with the costs of care from payers to providers. A wide variety of payment models based on such risk transfer have been proposed and tried over the years. These models provide a spectrum of options for ACO agreements – both on the public (Medicare/Medicaid) and the commercial (private payer) side. To understand what tools ACOs may need to manage new risks, we need to look at the kinds of risk ACOs assume. There are essentially two types of risk healthcare providers may share with payers: technical, or performance risk, and actuarial or insurance risk. In most pay-for-performance (P4P) programs, including Meaningful Use, providers are only required to assume performance risks. This is certainly true when P4P metrics are primarily process oriented (i.e., when providers are evaluated based on their ability to deliver consistent, recommended care processes). Patient outcomes, if ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 3
- 4. measured, are typically risk adjusted to protect providers from insurance risk. This, for example, is the case with the upcoming Medicare Value-Based Purchasing (VBP) Program. To manage performance risk, ACOs need the tools to manage their performance. Metrics of performance may vary, but generally include structure, process and outcome measures. Structure measures may include specific IT tools. For example, the proposed Medicare Shared Savings Program (MSSP) calls for a certain percentage of providers within the ACO to have adopted certified electronic health record (EHR) technology. Process measures are typically tied to evidence-based guidelines. To manage the performance across their provider network, ACOs need tools to implement guidelines, and to measure and improve their compliance. EHR technology provides the foundation, but may need to be augmented with clinical decision support and clinical data analytics tools. To manage patient outcomes, ACOs must also provide coordinated, patient-centered care. ACOs need tools to coordinate care, manage care transitions, manage medications and engage patients. Clinical data analytics tools need to provide reports that cover patients through the continuum of care. This implies EHR interoperability across the ACO network. Health information exchange (HIE) technology may be needed to integrate patient data within the provider network and beyond. A consolidated clinical data repository should be considered as the foundation for the analysis of care patterns and quality reporting. Disease registries may also be used to cover specific patient populations. Population health management tools will help ACOs design care protocols to improve patient outcomes. The Medicare Shared Savings Program (SSP) goes a step beyond P4P. To succeed under this program, ACOs must reduce the average cost of care under a predetermined benchmark. In this case too, risk adjustment is designed to protect providers from insurance risks. But beyond performance risk associated with achieving patient outcomes, this program requires providers to assume risks for cost. This implies that ACOs need tools to manage resource utilization. Ideally, these tools will be integrated with the analytical tools mentioned above. Initially, providers may work with payers to share the same tools payers are using for utilization management. It is only in the absence of risk adjustment or with capitation payment models that ACOs will be required to assume full risks for the cost of care, including insurance risks. To do that, ACOs will need the toolset of managed care organizations. For most ACOs, this will not be a viable option in the early stages. 5. What IT strategy can help deal with ACO unknowns? The health reform law has left many unknowns around the ACO model. Some of these are expected to clear over time. Yet other unknowns may purposely remain to allow for market innovation. Indeed, well ahead of the pilot demonstration projects mandated to begin by 2012, many private payers, provider groups and associations have already proposed or launched pilot projects. Models for these pilots vary greatly. Such great variation and flexibility in the ACO model implies the need for elasticity and agility in the ACO strategic plan, which in turn suggests that the same qualities will be required of its IT infrastructure. ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 4
- 5. ACOs should develop an IT strategy that enables them to respond quickly and effectively to changing market requirements and dynamics. Interoperable, standards-based systems will allow ACOs more choice in their selection of IT vendors and applications. In the next few years, ACOs should consider best-of-breed solutions to cover gaps in their current IT infrastructure. Many of the tools needed to succeed under the ACO model will also support other value-based payment models. As they build their IT infrastructure, ACOs should consider foundational tools that will benefit their members across multiple programs and payment models. 6. What are the key challenges ACOs face in redesigning care processes? As the care delivery system shifts from volume to value-based payment, ACOs are called upon to redesign care delivery around these new metrics. This is a tall order. To succeed, ACOs must embark on a journey very few healthcare organizations have attempted. And even the few who have – mostly large integrated delivery systems – can provide little useful evidence to the vast majority of our healthcare system, consisting of small uncoordinated fragments. Moreover, the scientific evidence base to guide this journey is highly incomplete, especially when it comes to cost. To meet the care process redesign challenge, ACOs must address multiple dimensions, including: • Reducing variation and disparities in care delivery among practices and individual providers, i.e. standardizing care. • Identifying the most effective care delivery processes to drive the organization’s strategic goals. • Identifying and implementing effective interventions to standardize care around the desired processes. • Leading cultural and behavioral change initiatives necessary to drive organizational change. • Developing a culture of learning and innovation that fosters on-going improvement, and the consumption, distillation and dissemination of best practices. • Centering care on patients and engaging them in the management of their own health. 7. How can IT help with the ACO’s care process redesign challenge? In their core function as agents of change, ACOs can find their best allies in information and the technologies that manage it. Recent events around the globe, such as the popular ousting of long- time rulers in North Africa, have provided dramatic and poignant proof of how information and technologies that facilitate its sharing on a massive and egalitarian basis can impact public opinion and affect drastic change. The same underlying principles are applicable to the ACO’s strategic goal of care process redesign and the organizational challenge inherent to it. Information that drives organizational change starts with data – timely, accurate, relevant and reliable data. Turning data into information requires technology. Technology enables aggregating and summarizing data. It supports analyzing data to identify actionable information. Technology allows visualizing data to drive action. With technology, data can be mined to gain new insights. Technology enables measuring performance and outcomes. Technology supports coordination and ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 5
- 6. collaboration. And it is through technology that knowledge can be most effectively collected and distributed. 8. What technologies can help ACOs redesign their care processes? To achieve their strategic goals, ACOs will need myriad IT tools. Many of these technologies are not new. They have been tried and proven in other industries. Some of them have been adopted in healthcare. But for the most part the application of these technologies to the ACO care process redesign challenge is new. And applying these tools to improve patient care will require breaking new ground. Among these technologies are the following: • Data analytics/business intelligence (BI) – Payers have used these tools for years to leverage claims data to manage health insurance risks more effectively. Some payers have even spun off businesses based on predictive modeling and data mining techniques. Many hospitals have used traditional BI tools to better manage their operations and finances. For ACOs, a new and exciting prospect is the integration of clinical data into these technologies. Arguably, such clinical business intelligence will be a critical success driver for ACOs. • Process management – Care delivery organizations have long applied process management methodologies to their business processes, such as supply chain and revenue cycle management. But the introduction of techniques like total quality management (TQM) to the process of care itself is relatively new and not commonly used today. To succeed in their mission to redesign care processes, ACOs will do well to adopt such technologies to their full potential. • Decision support – While many clinical decision support tools, such as order sets, medication safety alerts, etc., are already in use today, few healthcare organizations have adopted comprehensive and integrated decision support toolsets. Without such toolsets, however, ACOs have little hope of standardizing care even in those areas where standardization is highly desirable. • Knowledge and learning – Perhaps more than any other industry to undergo process redesign to date, healthcare faces this dual challenge: while medical knowledge is growing exponentially, much uncertainty remains along the care delivery process. Successful ACOs (and any healthcare providers) must embrace tools to manage and apply knowledge from both outside and internal sources and promote learning at both the individual and organizational levels. • Collaboration – Beyond the care coordination tools described above, collaborative technologies can help ACOs identify, distill and disseminate best practices within their network and across ACO networks. More than any other tool, collaborative technologies can accelerate the transformation required of ACOs. 9. What are the ACO’s unique organization management needs? Budgeting & Cost Accounting ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 6
- 7. Creating and operating an ACO can be more complicated than a traditional provider organization. Planning, upstart costs, arranging relationships with partners, interfaces to partner systems, staffing increases, expanding owned interests, and coordinating contracts, payments, and shared savings are just some of the major concerns that will require additional budgeting and cost accounting. In particular, payments to partners can be complex. Contract & Legal Management ACOs by their nature will require contracting with a broad range of partners with varying degrees of affinity. From close to loosely affiliated partners, contracts and legal management will be required. It’s also likely that ACOs will have to continually evolve to address changing business conditions, regulations, competition, payment reform and population health. As such, some partnerships may decrease or terminate while new ones may start or grow. Terminating partnerships early may lead to penalties. Partner organizations that do not meet their goals may also need to be pursued from a legal perspective to recoup costs, collect penalties, etc. In short, ACOs will be complex businesses with complex legal needs. Operational Management Running an ACO on a day-to-day basis will require a firm handle on revenue, expenses, resources, timing, etc. Provider organizations not experienced with managing risk and patient populations will need new skills and systems. Meeting reporting requirements, managing partners, ensuring government compliance, and doing so all in a timely fashion that meets stringent regulations and oversight will be key. Network Capacity They say that the biggest challenge for any business can be dealing with “success” – scaling up to new volumes and demands – while meeting customer and partner expectations. How big an ACO can grow in a fashion that is sustainable and meeting the needs of key stakeholders must be considered. Operational Benchmarking Any business can be compared on a relative and absolute scale. Particularly in the case of ACOs where success and shared savings will be based on comparison to peers, it will be crucial to understand how the organization stacks up. Success will require pushing into new areas of performance, including quality-based, speedier, cost-effective and innovative care. Benchmarks are a solid approach for comparing to others, and along with metrics and goals, can help an organization stay focused on the right direction. 10. What does an ACO need to do to engage patients? Among the requirements of Medicare ACOs are the following: • Create processes to promote evidence‐based medicine and patient engagement, report on quality and cost measures and coordinate care using telehealth, remote patient monitoring, etc.; and ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 7
- 8. • Meet patient‐centeredness criteria such as the use of patient and caregiver assessments or individualized care plans. For the purposes of this discussion we have used the following definitions: Patient engagement means engagement in one’s own health, care and treatment and involvement in the design, planning and delivery of health services. Patient-centeredness is defined as: "Health care that establishes a partnership among practitioners, patients, and their families (when appropriate) to ensure that decisions respect patients' wants, needs, and preferences and that patients have the education and support they need to make decisions and participate in their own care."1 Why is patient engagement important? There is a proven association (Coulter and Ellins 2006)2 between the engagement of patients in their health, care and treatment and the outcomes in relation to: • Patients’ recall of information, knowledge and confidence to manage their conditions; • The likelihood of patients reporting that the chosen treatment path was appropriate for them; • Patient reports of their experiences, and of their satisfaction with care; and • Use of healthcare resources, where engaged patients are more likely to adhere to chosen courses of treatment, and to participate in monitoring and prevention. It has also been shown that some interventions to involve patients in sharing the decision over treatment choice result in patients choosing less interventionist (and costly) treatments than their clinicians might otherwise have recommended. Judith Hibbard, a professor of health policy at the University of Oregon, noted patients usually encounter a one-size-fits-all provider approach when it comes to finding ways for them to manage their chronic conditions. However, if providers had more information on their patients' abilities to engage and self-manage their conditions, they might be better able to target and support a patient's healthcare needs, she said. "We've found that tailoring support to the patient's level of [engagement] is an important way to help [patients] become more activated and to be able to do all the behaviors we're asking them to do," she said. Hibbard and her colleagues developed a measure to assess skill, confidence, and knowledge among patients about managing their conditions. With the measurement, they've been able to find new ways "to actually do a better job of engaging people." The degree of patient engagement in consultations can be measured through patient experience reports. ACOs depend on more informed and engaged patients who assume more financial risk to help meet the goals of lower costs, higher quality, and greater satisfaction. The Internet's advances and methods for secure access make true patient engagement a reality. ACOs will have to create portals where patients can access information about their wellness and health status such as lab results or pharmacy prescriptions, and reliably compare treatments, specialists, hospitals and costs. ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 8
- 9. The Society of Participatory Medicine proposes the following processes to promote patient engagement and centeredness. Patient engagement • Working with patients to identify and minimize barriers to timely and effective action by patients. • Involving patients with central, meaningful roles in practice improvement efforts, such as quality improvement teams • Creating a patient advisory council with adequate resources and meaningful access to ACO leadership. • Implementing mechanisms for regular assessment (at least annually) and improvement of patient engagement standards and processes. Patient-Centeredness • Collaborating with patients to ensure that they have the knowledge, skills and support to make informed decisions about their care as providers and patients work together to achieve the patients’ aims. • Maintaining and enforcing policies that ensure the provision of clear explanations and availability of individuals’ information about their health and healthcare while guarding the privacy of this data. • Maintaining and enforcing policies that facilitate and encourage individuals’ full engagement and participation in their care, but do not require it. Such polices shall include, without limitation, the following: (a) Offer open scheduling and extended office hours: (b) Create reminders for patients and providers, delivered by means selected by the individual; (c) Provide direct patient access to health data; (d) Otherwise use technology as appropriate to facilitate meaningful patient and family participation in care; and (e) Provide transparent information about services, their cost, and insurance coverage. 11. How to Measure Patient Engagement and Patient Centeredness? While the Institute for Healthcare Improvement (IHI) has defined three objectives of their Triple Aim strategic initiative (to improve patient experience, the population’s health and medical costs), the measures used to evaluate progress along those domains have not been prescribed. The IHI Triple Aim prototyping participants around the world have each developed individual approaches to establishing their Triple Aim measures of success. ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 9
- 10. Managed care organizations have significant experience with understanding the needs of their patient populations. Using a variety of analytic techniques, managed care leaders continuously assess the costs of care, quality of care metrics, and the relative efficiency and quality of care provided by individual providers. The ACO environment offers an opportunity for leaders to apply lessons learned about assessing population needs from the managed care experience. In addition to assessing needs through claims and EHR data, leaders must gather relevant information to allow them to understand the language, cultural, and social needs of the ACO population. Only by understanding the true needs of the population can ACO leaders prioritize the activities that will have the most impact on improving the health of the population. The National Healthcare Quality Report (NHQR) tracks four measures of the patient experience of care. The core report measure is a composite of these measures: (1) patient assessments of how often their provider listened carefully to them; (2) explained things clearly; (3) respected what they had to say; and (4) spent enough time with them. In addition, the 2007 NHQR presents four composite supplemental measures from the Hospital Consumer Assessment of Healthcare Providers and Systems (H-CAHPS), the hospital version of CAHPS® that focus on the quality of communication that patients experience during their hospital stay. This is important not only because effective patient-provider communication can help ensure that medical decisions are consistent with the patient's needs and preferences, but also because patients can help providers avoid problems with medications and problems that may arise after they are discharged. The NHQR includes one core measure of patient centeredness—a composite measure on the patient experience of care—and two new supplemental measures. Because having a diverse workforce of healthcare providers may be an important component of patient centered health-care for many patients, the report includes a new supplemental measure of workforce diversity— race/ethnicity of the nation's registered nurse (RN) workforce. A supplemental measure focusing on health literacy of U.S. adults is also presented. Measuring Patient Engagement / Satisfaction ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 10
- 11. The Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys are widely used, rigorously designed, and available in formats that can be used to assess a variety of experiences, including inpatient stays, home healthcare, interactions with health plans, and accessing pediatric care. Of the available surveys of patient satisfaction across the continuum of care, only the CAHPS instruments have been widely used and have benchmarking data available. For more information, see Press Ganey surveys, Consumer Assessment of Healthcare Providers and Systems (CAHPS) surveys and/or the Health Resources and Services Administration’s Health Center Patient Satisfaction Survey [http://bphc.hrsa.gov/patientsurvey]. 12. What are some of the tools that support patient engagement? 1. Individualized care plans are established processes in place to include patients and their family members as part of the care team and to ensure that care plans are customized for the individual’s needs and desires. Individualized care plans: • Ensure that the patients’ needs (e.g., readiness for change) are understood and that their personal goals and values are taken into account. • Ensure that both general health goals (e.g., relief of depression symptoms) and clinical goals (e.g., normalizing blood pressure) are integrated into the care plan and prioritized according to the patient’s values. A template for an individualized care plan can be embedded in the EHR and shared with the patient either in hard copy or electronically. Care management systems that can pre-populate a draft care plan with recommended goals and an action plan; can be designed to incorporate data from a variety of sources (e.g., lab data etc.) and use clinical logic to prioritize risk factors. Ideally, individualized care plans are member-centric, not provider-centric, and are thus are shared across a health system so each patient has one care plan. 2. Patient decision support system involves having mechanisms in place for patients to access comprehensive information about their condition and treatment options and to receive help in discerning and communicating their preferences and values. Such systems need to use existing tools within the healthcare system as part of a proactive, creative process to engage patients in their healthcare through a variety of tools and approaches (e.g., reminder systems, protocols for follow-up, action steps used to shift people’s thinking about their care, outreach by social workers and case managers, increasing transparency with a patient’s individual health information). 3. Patient portal for electronic information access via the Internet to a wide variety of information provided centrally by the ACO; provides people with access to several of the other operating activities within the people-centered foundation. One of the most important barriers to the use of patient portals is lack of access to or comfort with electronic media. For this reason, significant marketing efforts are needed to achieve uptake. Portals associated with health plans have historically had exceptionally low adoption rates, possibly due to the tendency for consumers to distrust health plans. Some of the patient portals crafted by health plans have excellent functionality and—despite the low uptake rates—may be useful prototypes for ACO leaders to consider. ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 11
- 12. Connection should be made with the communication and marketing departments of the healthcare systems, payers and employers to develop a patient portal that will best engage patients and to create messages that promote the understanding that the goal of people-centered care within the ACO is to give people more control, not to shift all responsibility from providers or restrict access to needed care. 4. Personal health record (PHR) is a computerized application that stores an individual's personal health information and provides the mechanism for access to that information. The PHR includes a record of a patient’s healthcare experience built from EHR, claims data, and other sources of information. One of the principle distinguishing features of a PHR is the platform by which it is delivered. The types of platforms include: paper, personal computers, the internet, and portable devices. References Berwick DM, Nolan TW, Whittington J. The Triple Aim: Care, Health, and Cost. Health Affairs, vol 27 no.3, 2008; 759-769. Berwick DM. What 'Patient-Centered' Should Mean: Confessions of an Extremist. Health Affairs, vol 28 no. 4, 2009; 555-565. Coulter A, Ellis J. Patient Focused interventions. A review of the evidence. Picker Institute Europe. 2006. Dixon A, Greene J, Hibbard J. Do Consumer-Driven Health Plans Drive Change in Enrollees’ Health Care Behavior? Health Affairs. 2008; 1120-1131. Fendrick AM, Chernew ME. Value-based Insurance Design: Aligning Incentives to Bridge the Divide between Quality Improvement and Cost Containment. American Journal of Managed Care. Vol 12, 2006; SP5 - SP10. Hibbard JH, Greene J, Tusler M. Improving the Outcomes of Disease Management by Tailoring Care to the Patient's Level of Activation. American Journal of Managed Care. No. 6,June 15, 2009; 353 - 360. Hibbard JH, Cunningham PJ. How Engaged Are Consumers in Their Health and Healthcare, and Why Does It Matter? Washington, DC: Center for Studying Health System Change. 2008. Institute for Healthcare Improvement. The Triple Aim- Optimizing health, care and cost. Healthcare Executive. Vol 24 no. 1, Jan/Feb 2009; 64-66. Institute of Medicine. Envisioning the National Health Care Quality Report. Washington, DC: National Academy Press. 2001. McGlynn EA, Asch SM, Adams J, Keesey J, Hicks J, DeCristofaro A, et al. The Quality of Health Care Delivered to Adults in the United States. New England Journal of Medicine. Vol 348 no.26, June 2003; 2635 - 2645. ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 12
- 13. Mittler JN, Landon BE, Fisher ES, Cleary PD, Zaslavsky AM. Market Variation in Intensity of Medicare Service Use and Beneficiary Experiences with Care. Health Services Research. Vol 45 no.3, June 2010: 647 – 669. National Committe for Quality Assurance. The State of Health Care Quality - Value, Variation and Vulnerable Populations. Washington, DC: National Committe for Quality Assurance. 2009. Saha S, Beach MC, Cooper LA. Patient Centeredness, Cultural Competence and Healthcare Quality. Journal of the National Medical Association. Vol 100 no.11,Nov 2008; 1275 – 1285. Solberg LI, Klevan DH, Asche SE. Crossing the Quality Chasm for Diabetes Care: The Power of One Physician, His Team, and Systems Thinking. Journal of the American Board of Family Medicine. Vol 20 no.3, 2007; 299 - 306. Wasson JH, Baker NJ. Balanced Measures for Patient-Centered Care. Journal of Ambulatory Care Management. Vol 32, no. 1, 2009; 44-55. Patient activation and engagement metric references: Hibbard JH, Mahoney ER, Stockard J, Tusler M. Development and Testing of a Short Form of the Patient Activation Measure. Health Services Research. 2005; 40:6: 1918-1930. Wasson JH, Bartels S. CARE Vital Signs Supports Patient-centered, Collaborative Care. Journal of Ambulatory Care Management. 2009; 32(1): 56-71. Safran DG, Karp M, Coltin K, Chang H, Li A, Ogren J, Rogers WH. Measuring Patients’ Experiences with Individual Primary Care Physicians: Results of a Statewide Demonstration Project. Journal of General Internal Medicine. 2006; 21:13–21. Authors Alan Gilbert VP Business Development, AxSys Technology Kenneth A. Kleinberg, FHIMSS Senior Director, The Advisory Board Company Kobi Margolin CEO, Clinigence Joe Pleasant, FHIMSS Senior VP & CIO, Premier, Inc. Edna Boone, CPHIMS HIMSS Staff Liaison ©2011 Healthcare Information and Management Systems Society (HIMSS) Page 13
