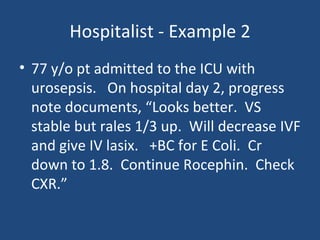
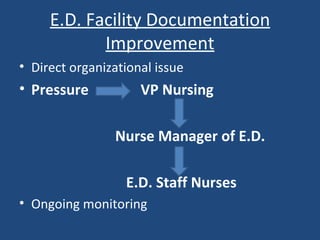
This document discusses the importance of clinical documentation improvement (CDI) programs in both inpatient and outpatient settings. It provides several examples showing how more thorough documentation can result in more accurate coding, higher reimbursement, and improved quality metrics. Key areas discussed include documentation for inpatient conditions, procedures, ED levels of care, physician E/M coding, and specialties like radiology, hospitalists, and pain clinics. The document emphasizes that comprehensive documentation is essential for accurate billing and reflects the complexity of care provided.