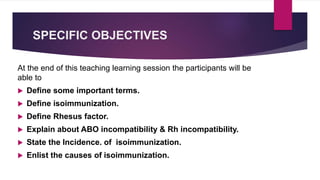
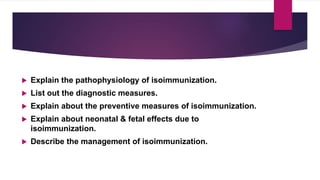
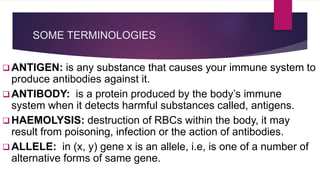
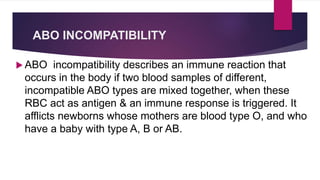
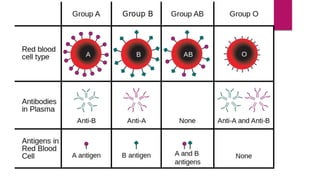
This document provides information about isoimmunization. It lists the group members presenting on the topic and includes the objectives of the presentation. It defines key terms and explains ABO and Rh incompatibility, causes of isoimmunization, pathophysiology, diagnosis, prevention, and management of maternal and neonatal isoimmunization. Nursing management is also described. References are provided.



![ HYDROPS FETALIS: Is a severe, life threatening
problem in which abnormal amounts of fluid build up
in two or more body areas of a fetus or a newborn.
SALINE AGGLUTININ[IgM]: This type of antibody is
1st to appear in the maternal circulation. They are
large molecules cannot pass through the placental
barrier & is not harmful to fetus.](https://image.slidesharecdn.com/isoimmunization-161202134714/85/Isoimmunization-10-320.jpg)
![ ALBUMIN AGGLUTININ[IgG]: It is also called incomplete
or blocking antibody. Because of its small molecule it can
cross the placenta barrier & cause damage to the fetus.
TITRE: is a laboratory test that measures the level of
antibodies in a blood sample.
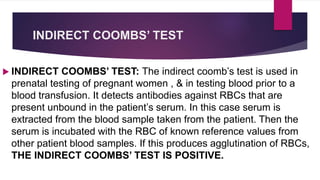
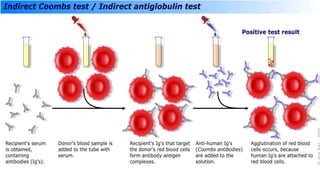
COOMBS’ TEST: Is used to detect antibodies that are
stuck to the surface of red blood cells.](https://image.slidesharecdn.com/isoimmunization-161202134714/85/Isoimmunization-11-320.jpg)
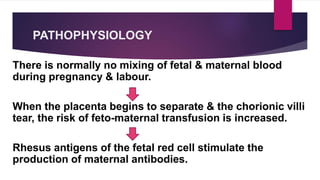
![Contd…
The first encounter may not result in actual antibody
formation but the women will be sensitized: on a second
encounter antibodies are produced in abundance. Once
formed there antibodies are permanent.
The antibody formed in the maternal system [IgG] crosses
the placenta barrier & enters into fetal circulation.](https://image.slidesharecdn.com/isoimmunization-161202134714/85/Isoimmunization-28-320.jpg)
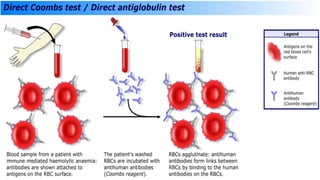
![DIRECT COOMBS’ TEST
The direct coombs’ is used to detect these antibodies or
complement proteins that are bound to the surface of RBC. A
blood sample is taken & the RBCs are washed & then
incubated with antihuman globulin[also known as coombs’
reagent]. If this produces agglutination [clumping together] of
RBCs, THE DIRECT COOMBS’ TEST IS POSITIVE.](https://image.slidesharecdn.com/isoimmunization-161202134714/85/Isoimmunization-36-320.jpg)

![MEDICAL MANAGEMENT OF
ISOIMMUNIZATION
ANTENATAL MANAGEMENT
• Detection of maternal sensitization.
Detection of maternal sensitization is confirmed by the detection of Rh
antibodies in maternal circulation, it is done by titre technique. Titre
below 4IU/ml are unlikely to produce severe fetal disease.
All Rh negative pregnant women should have their blood tested for Rh
antibodies at the 1st antenatal visit and again at 28th & 34th weeks of
gestation. .[acc. To DC Dutta, textbook of obstetrics, 16th edition]](https://image.slidesharecdn.com/isoimmunization-161202134714/85/Isoimmunization-49-320.jpg)
![Contd…….
• Management of affected fetus by intrauterine intravascular
transfusion.
Blood may be given to the baby by a needle introduced through
mothers abdomen. Blood is given either intravascularly [into the
umbilical vein] or intraperitoneally.
The first method is preferable, as blood enters the fetal
circulation directly and severely anemic fetuses may be saved.](https://image.slidesharecdn.com/isoimmunization-161202134714/85/Isoimmunization-50-320.jpg)