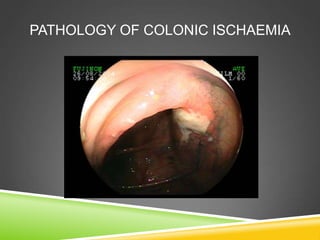
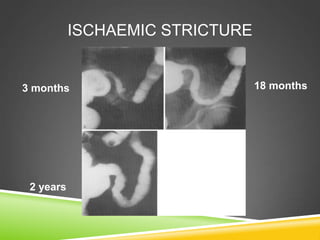
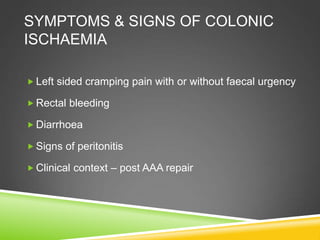
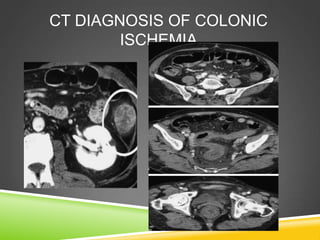
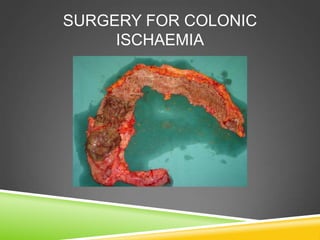
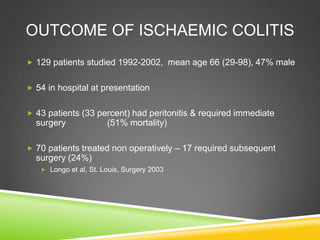
Ischaemic colitis is a common condition in the elderly and can range from transient inflammation to severe gangrene, with its true incidence often underestimated. Predisposing factors include vascular occlusions, low blood flow states, and hypercoagulable conditions, while symptoms typically present as left-sided cramping, rectal bleeding, and diarrhea. Management may involve supportive care and regular assessments, with surgery indicated for severe cases showing signs of peritonitis or infarction.