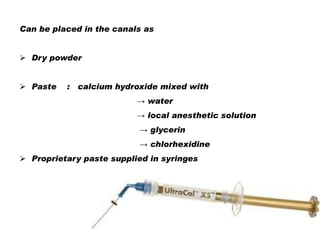
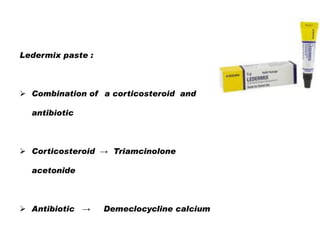
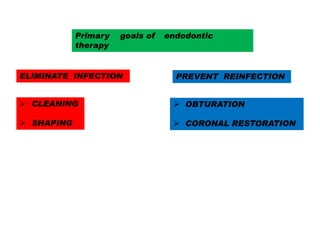
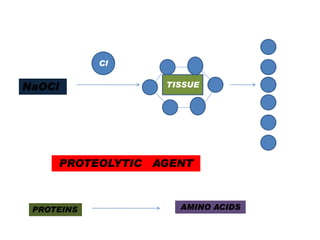
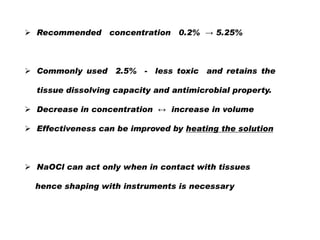
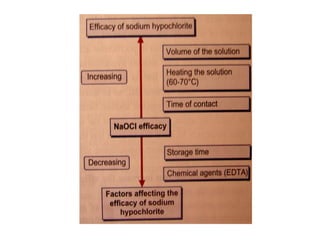
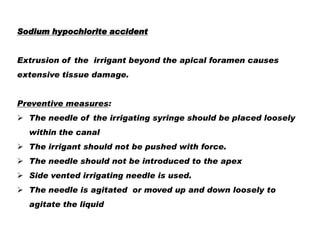
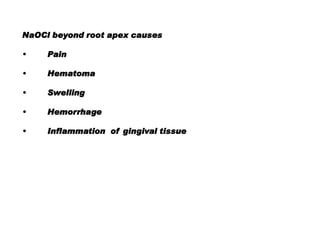
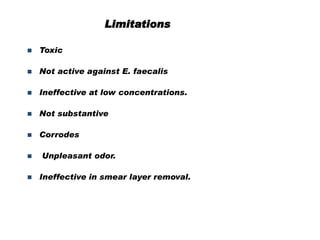
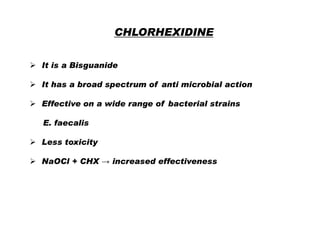
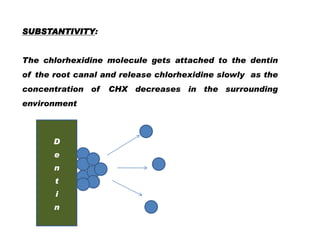
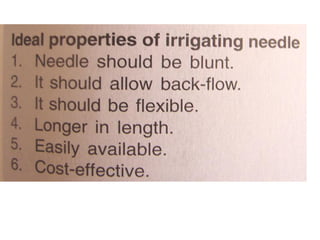
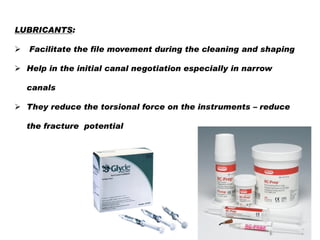
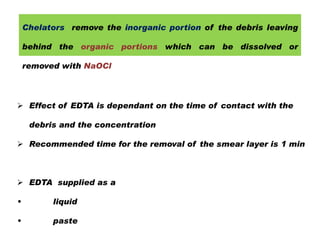
The document discusses irrigants and intracanal medicaments used in endodontic therapy. The goals of endodontic treatment include eliminating infection, preventing reinfection through cleaning, shaping, obturation and coronal restoration. Sodium hypochlorite and chlorhexidine are commonly used irrigants that have antimicrobial properties. Chelating agents like EDTA are used to remove the smear layer formed during instrumentation. Calcium hydroxide is a widely used intracanal medicament due to its high alkalinity and antimicrobial effects. Combination medications containing corticosteroids and antibiotics can also be used to reduce pain and prevent bacterial overgrowth.
![SODIUM HYPOCHLORITE
[ NaOCl ]
Commonly used household bleach [ Clorox ]
Most common and popular irrigant in endodontics
Advantages:
Mechanical flushing of debris from the canal
Tissue dissolving capacity → Vital + Non vital [necrotic]
Antimicrobial action
Lubrication
Inexpensive
Easily available](https://image.slidesharecdn.com/irrigation-140121154045-phpapp02/85/Irrigation-9-320.jpg)
![Anti microbial action :
Adsorption to the surface of bacteria [due to cationic-anionic
electrostatic attraction]
Increase the membrane permeablility
Results in micro leakage of intracellular components leading
to cell death
CHX](https://image.slidesharecdn.com/irrigation-140121154045-phpapp02/85/Irrigation-17-320.jpg)
![OTHER IRRIGATING SOLUTIONS
HYDROGEN PER OXIDE
[ H2O2 ]
It is an oxidizing agent .
It is almost used in conjunction with NaOCl
It acts by two mechanisms
1. The reaction with NaOCl produces effervescence
which mechanically pushes the debris out of the
canal
2. The nascent oxygen released acts as a powerful
antimicrobial agent especially for the anaerobic
organisms](https://image.slidesharecdn.com/irrigation-140121154045-phpapp02/85/Irrigation-22-320.jpg)
![Ultrasonics [passive ultrasonic irrigation]
Most of the dentine debris is inorganic
matter that cannot be dissolved by
NaOCl. Therefore, removal of dentine
debris relies mostly on the flushing
action of irrigant.
The ultrasound device allow the
endodontic irrigant to pass along the
ultrasonic files. The irrigant is activated
by the ultrasonic energy imparted from
the energized instruments producing
acoustic streaming and cavitation](https://image.slidesharecdn.com/irrigation-140121154045-phpapp02/85/Irrigation-27-320.jpg)
![Commonly used lubricants;
Glycerin
Glycol + urea peroxide + EDTA
EDTA 19% + 10 %
GEL]
[ RC PREP]
carbamide peroxide [DOLO ENDO](https://image.slidesharecdn.com/irrigation-140121154045-phpapp02/85/Irrigation-29-320.jpg)
![DECALCIFYING / CHELATING AGENTS
Agents that dissolve or dissolute the inorganic portions of the
root dentine [ calcified portions]
Ethylene di-amine tetra acetic acid [ EDTA]
Helps in the removal of the smear layer
Irrigation with 17% EDTA followed by the final rinse with
NaOCl is recommended](https://image.slidesharecdn.com/irrigation-140121154045-phpapp02/85/Irrigation-33-320.jpg)
![MTAD [ BIOPURE MTAD]
MTAD was developed by Mohmand Torabinajed et al
MTAD contains mixture of :
•
tetracycline isomer doxy cycline
•
acid- citric acid
•
a detergent - Tween 80
Antimicrobial activity of MTAD
MTAD has superior antimicrobial activity than 5.25% sodium
hypochlorite. The efficiency of MTAD in disinfecting surface of
the roots is a result of the presence of doxycycline.](https://image.slidesharecdn.com/irrigation-140121154045-phpapp02/85/Irrigation-35-320.jpg)

![PHENOLICS
ALDEHYDES
Eugenol
Formocresol
Camphorated monoparachloro phenol
Glutaraldehyde
[CMCP]
Parachlorophenol [PCP]
HALIDES
Camphorated parachloro phenol [CPC]
Sodium hypochlorite
Metacresylacetate
Iodine – potassium iodide
Cresol
Creosote [ beechwood]
Thymol
STERIODS
CALCIUM HYDROXIDE
ANTIBIOTICS
COMBINATION](https://image.slidesharecdn.com/irrigation-140121154045-phpapp02/85/Irrigation-38-320.jpg)
![Physico-chemical properties
pH
Viscosity [Viscosity changes over time ]
Adhesion
Solubility
Radio-opacity
Working time
Sealing ability](https://image.slidesharecdn.com/irrigation-140121154045-phpapp02/85/Irrigation-40-320.jpg)