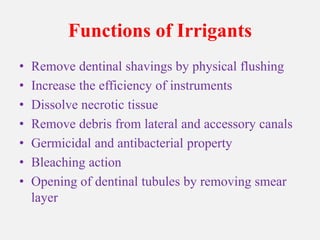
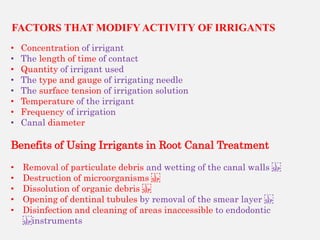
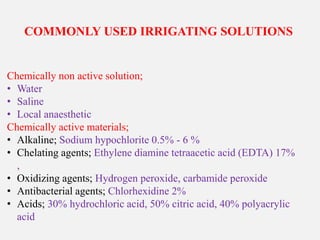
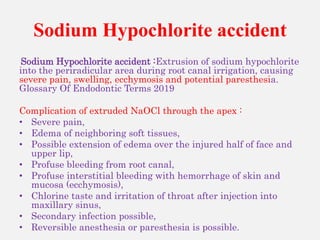
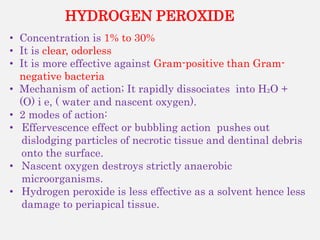
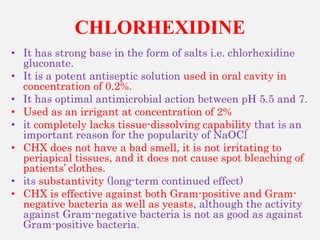
This document discusses root canal irrigants. It begins by outlining the objectives and functions of irrigants, which include removing tissue, microorganisms, and debris from the root canal. It describes the ideal requirements for an irrigant and commonly used irrigating solutions such as sodium hypochlorite, hydrogen peroxide, chlorhexidine, and chelating agents like EDTA. The mechanisms of action, advantages, and disadvantages of different irrigants are provided. Factors that influence irrigant activity and how to increase the efficacy and safely use sodium hypochlorite are also summarized.