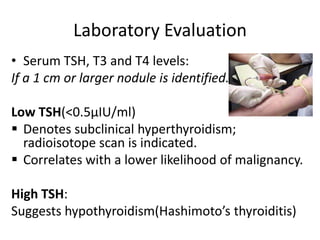
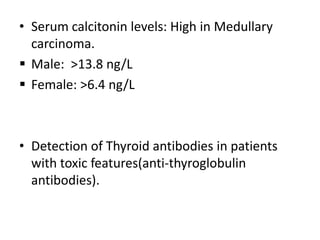
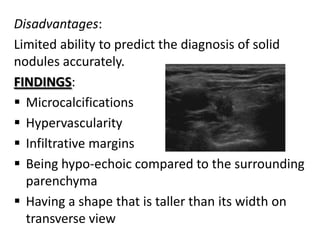
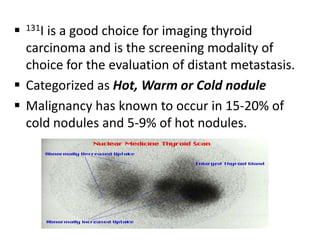
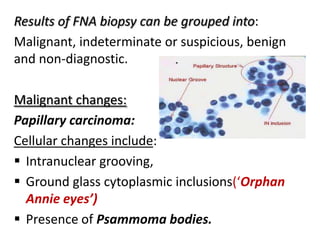
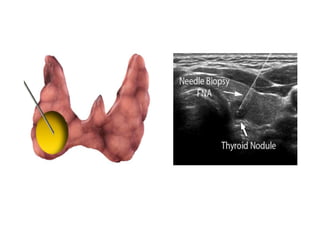
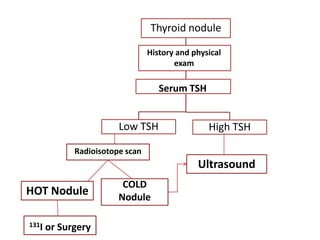
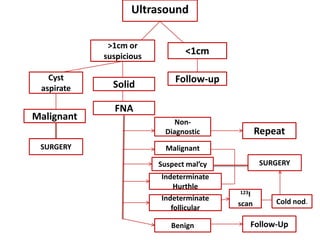
This document discusses the various investigations used to evaluate thyroid nodules. Laboratory tests like serum TSH, T3, T4 and calcitonin levels provide information about thyroid function. Ultrasound is used to determine nodule size, characteristics and detect lymph nodes. Radioisotope scanning assesses thyroid function and categorizes nodules as hot, warm or cold. Fine needle aspiration biopsy is the key modality for evaluation, with results categorized as malignant, indeterminate, benign or non-diagnostic. Computed tomography or magnetic resonance imaging can evaluate local extension in advanced thyroid cancer. The algorithm outlines evaluation and management based on test results.