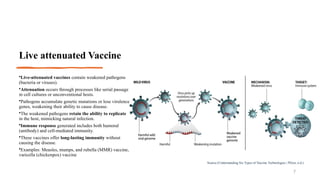
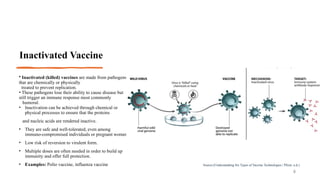
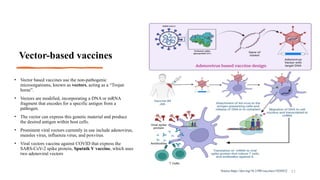
The document provides an overview of vaccines, explaining their definition, historical significance, and types, including live attenuated, inactivated, subunit, toxoid, vector-based, and nucleic acid vaccines. It highlights how vaccines function by inducing an immune response and how they exploit the human immune system's ability to remember pathogens. The historical context notes early contributions from figures like Edward Jenner and Louis Pasteur in the development of vaccination techniques.





![Nucleic acid vaccines
• Nucleic acid-based vaccines, including DNA (as
plasmids) and RNA [as messenger RNA (mRNA)]
encode for pathogen-specific antigenic proteins.
• DNA vaccines are generated by inserting a gene
encoding antigens into a bacteria-derived plasmid.
• DNA vaccines, after internalization, the DNA is
transferred to the nucleus for transcription and then
translated in the cytoplasm.
• Unlike DNA vaccines, RNA vaccines allow direct
translation of the antigen within the cytoplasm.
• RNA vaccines can effectively carry antigen-encoding
mRNA to APCs directly in vivo ( via nanocarriers).
• Examples: Against COVID-19 : Comirnaty® (Pfizer-
BioNTech vaccine). Spikevax® (Moderna vaccine)
12
Source: https://doi.org/10.1038/s41573-021-00283-5](https://image.slidesharecdn.com/vaccinesanditstypes1-241128112139-03656329/85/Introduction-to-Vaccines-and-it-s-classification-12-320.jpg)
