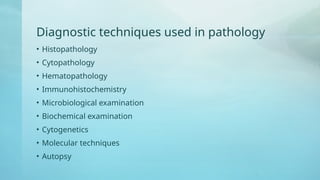
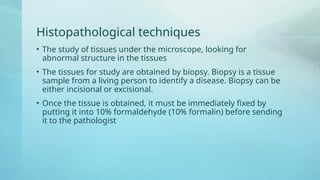
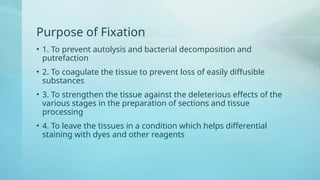
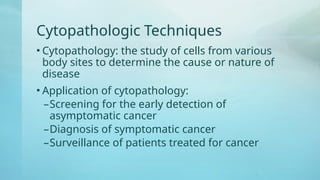
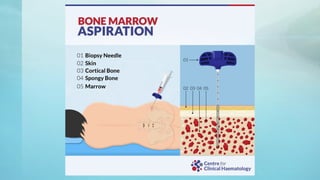
The document provides an overview of pathology, defining it as the scientific study of disease, including its etiology, pathogenesis, morphologic changes, and clinical significance. It details various diagnostic techniques used in pathology, such as histopathology and cytopathology, and highlights the course and outcomes of diseases. Additionally, it discusses the causes of disease and distinguishes between clinical and biological death.