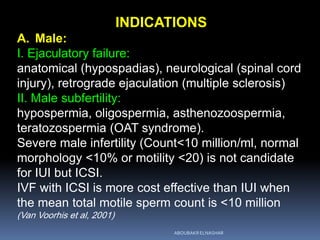
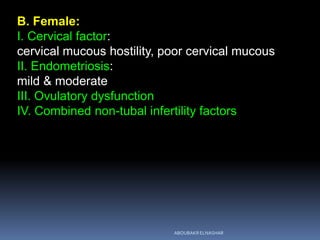
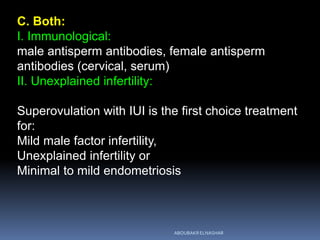
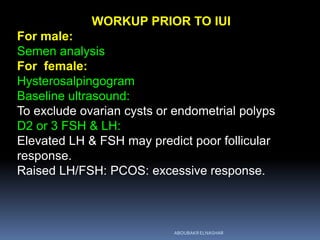
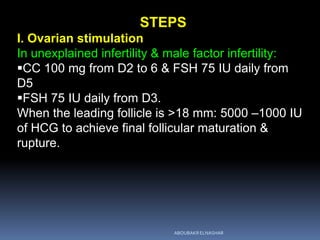
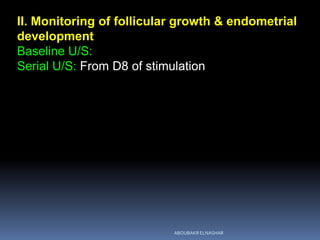
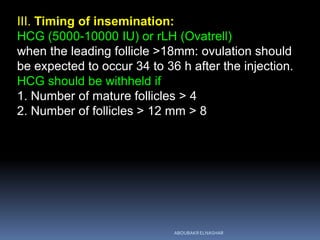
This document outlines the protocol for intrauterine insemination (IUI). It describes the indications for IUI including male factor infertility and various types of female infertility. It details the workup that should be done prior to IUI including semen analysis and ultrasound exams. The steps of the IUI process are explained, including ovarian stimulation when needed, follicle monitoring, sperm preparation techniques, timing of insemination, and the insemination procedure. It recommends offering 4 to 6 cycles of IUI.