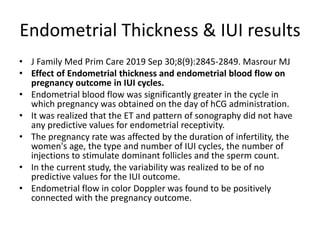
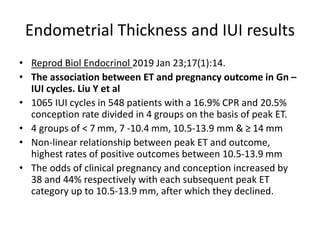
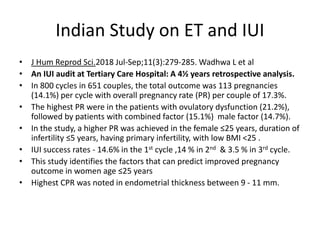
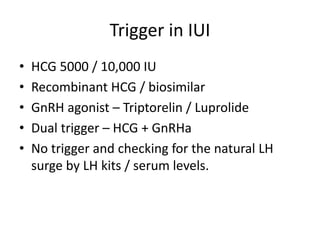
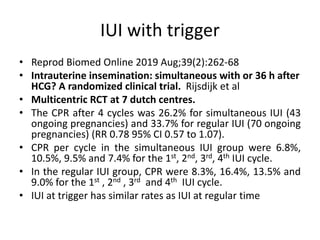
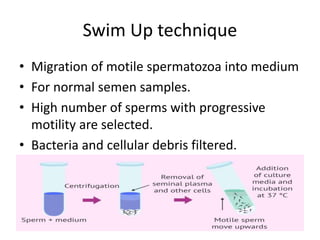
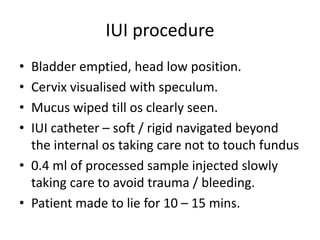
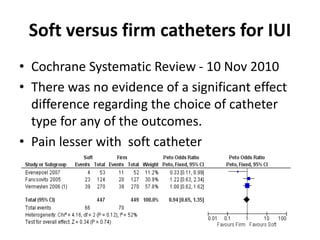
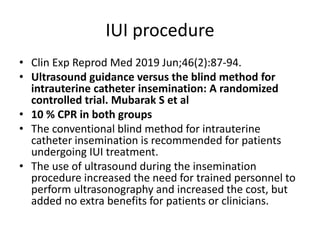
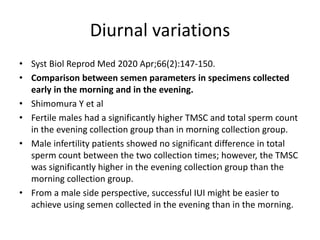
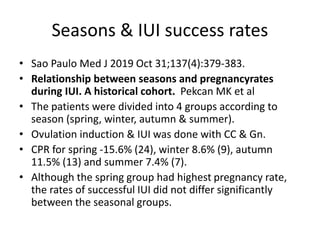
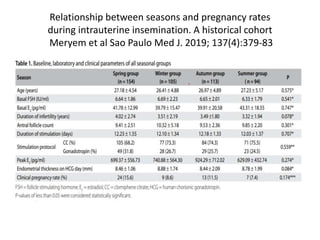
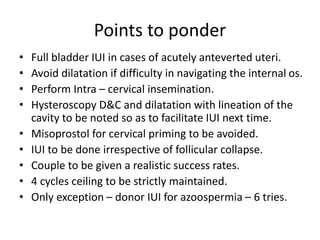
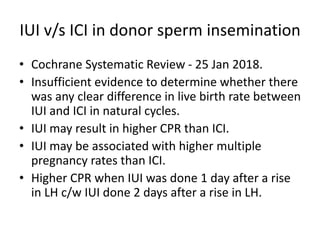
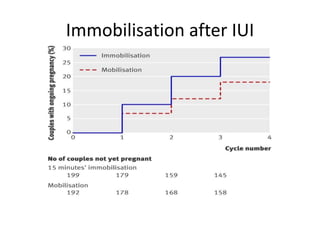
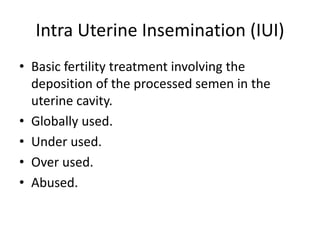
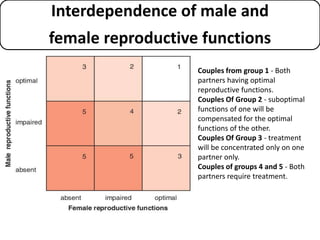
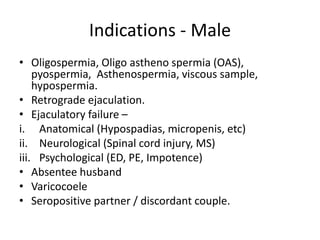
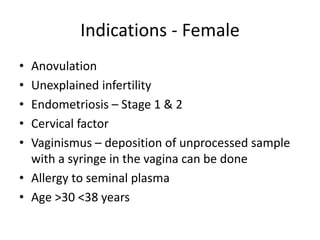
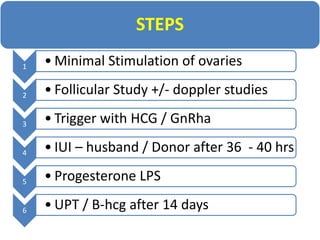
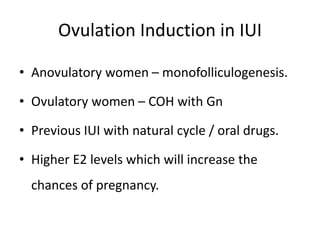
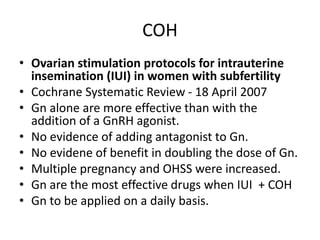
The document discusses intrauterine insemination (IUI) as a key fertility treatment, detailing its indications, contraindications, and the procedures involved. It highlights the success rates of IUI compared to IVF, the importance of ovarian stimulation protocols, and the role of semen washing in improving outcomes. Additionally, it presents research findings on factors affecting IUI success, such as endometrial thickness, follicular phase length, and the effectiveness of various trigger methods for ovulation.
![• Arch Gynecol Obstet 2019 Dec;300(6):1767-17, Kaur J et al
• Prospective randomized trial comparing letrozole step-up protocol with
letrozole + Gn for COS & IUI in patients with unexplained infertility.
• Group A COS was done by step-up protocol of letrozole from day 2 or 3 of
menstrual cycle, starting with 2.5 mg and increased to 5, 7.5, 10 mg.
• Group B Letrozole 2.5 mg BID was given for 5 days and IM hMG 150 IU was
given every alternate day from day 7 and titrated according to response.
• HCG was given when leading follicle was 17 mm and IUI > 36 h.
• Ovulation rate of 90.9% (40/44) in group A, 100% (55/55) in group B.
• CPR / Pt , 3/28 (10.7%) in group A versus 5/30 (16.67%) in group B. (NS)
• The mean (SD) cost of medicines was significantly lower in group A Rs.
345.00 (00) compared to group B Rs. 2148.64 (515.67) [p < 0.0001].
• It is possible to achieve multifollicular development with use of letrozole
step-up protocol, even without addition of Gn, at significantly lower cost.](https://image.slidesharecdn.com/iui-newerconcepts-200410103034/85/Iui-newer-concepts-16-320.jpg)