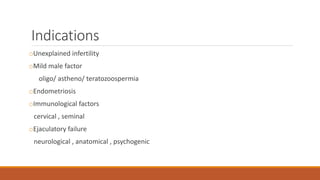
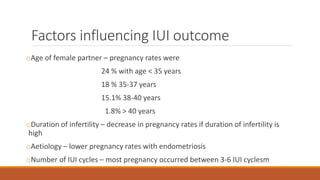
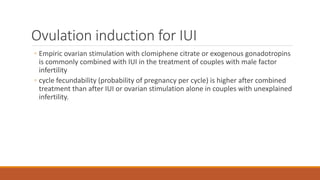
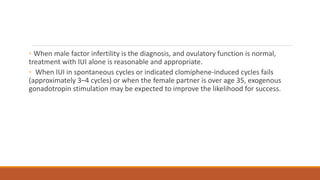
Intrauterine insemination (IUI) is a fertility treatment involving the placement of washed sperm into the uterine cavity and is indicated for various infertility causes, excluding tubal disease. Success rates vary based on factors such as female age and sperm quality, with combined treatments showing higher pregnancy rates than IUI alone. Proper timing of IUI and effective sperm preparation methods are crucial for maximizing the chances of conception.




![Donor Sperms
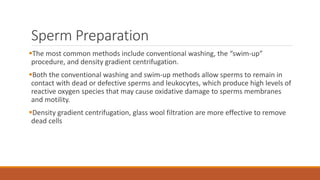
Require extensive screening of prospective sperm donors before acceptance.
Semen quality, to include an evaluation of sperm viability and motility after a trial
freeze and thaw, excludes approximately 75% of all candidates.
Personal health history and physical examination, family medical history, genetic
screening for cystic fibrosis and other carrier states (depending on ethnicity),
Screening for sexually transmitted infections (syphilis, gonorrhea, Chlamydia,
cytomegalovirus, hepatitis B and C, HIV types I and II, and human T-lymphocytic
virus [HTLV] types I and II](https://image.slidesharecdn.com/intrauterineinsemination-240626150750-e1df47af/85/Intrauterine-insemination-techniques-17-320.jpg)