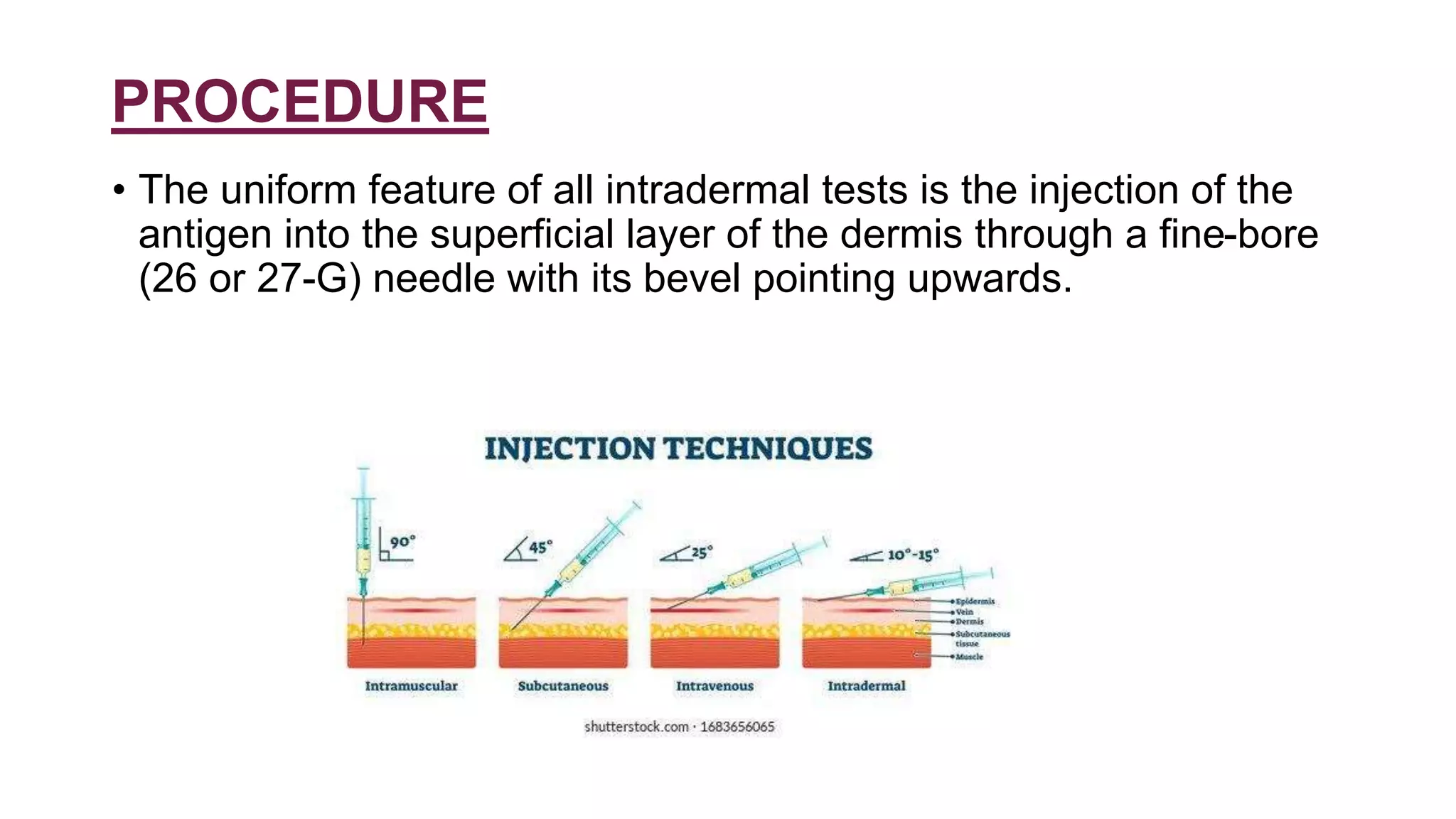
The document provides information about intradermal tests. It defines intradermal tests as tests that involve injecting small amounts of diluted antigens into the skin. The document discusses the procedure for performing intradermal tests and interpreting the results. It also describes several specific intradermal tests used to diagnose infectious diseases like tuberculosis, leprosy, fungal infections, and parasitic infections as well as non-infectious conditions.