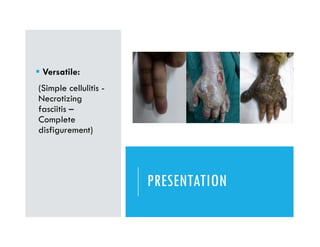
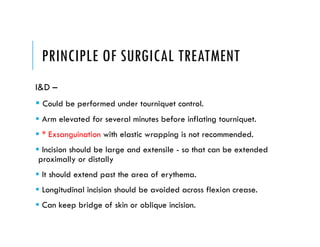
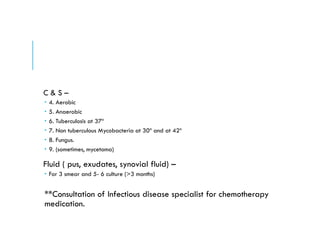
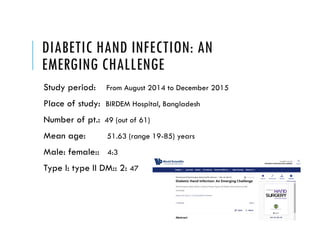
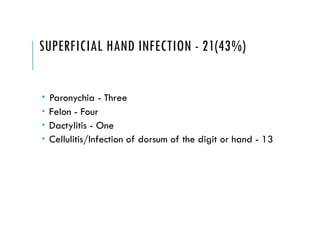
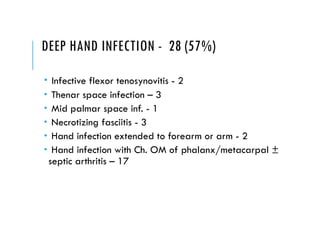
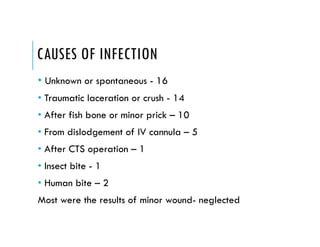
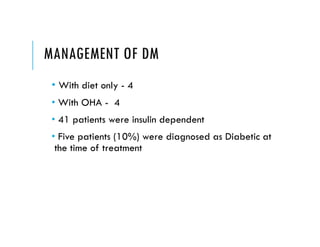
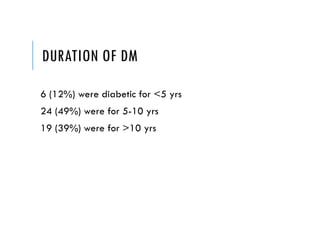
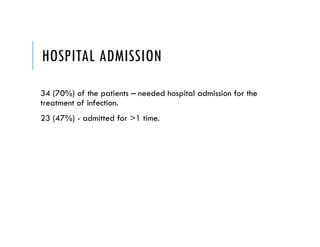
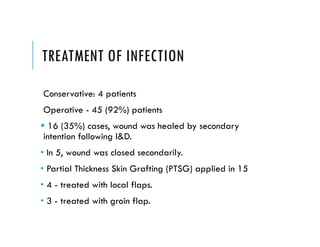
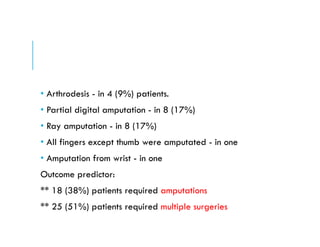
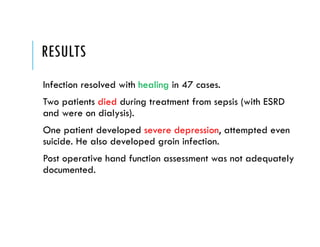
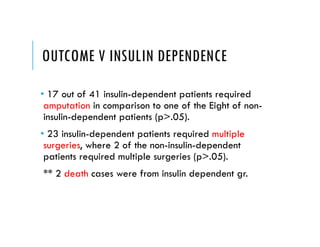
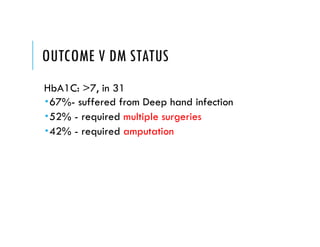
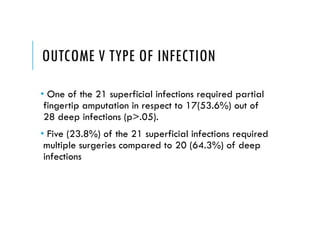
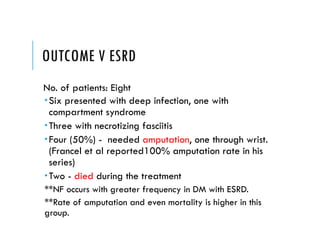
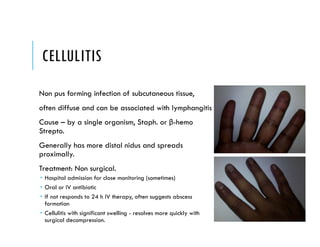
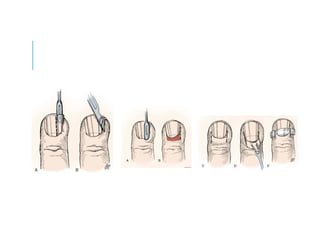
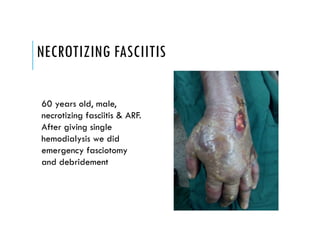
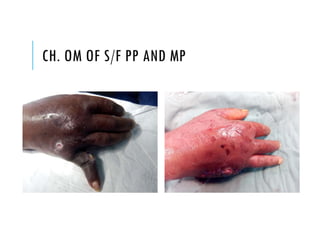
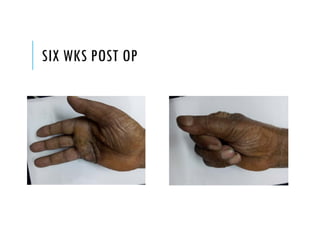
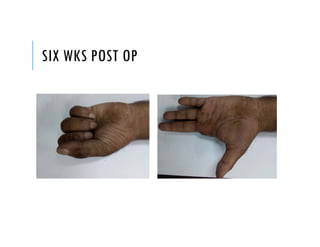
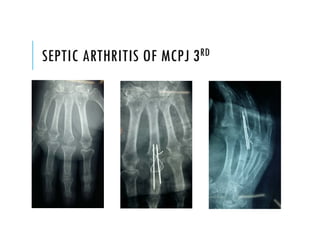
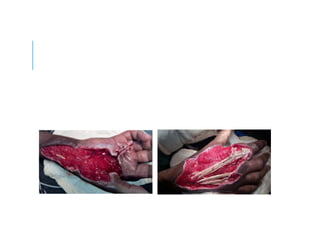
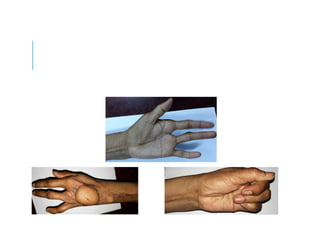
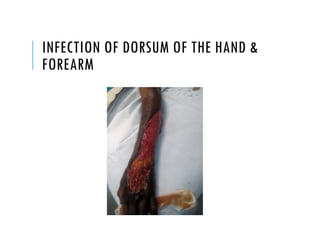
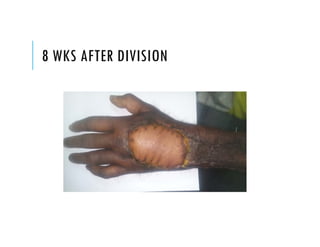
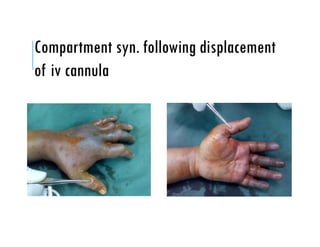
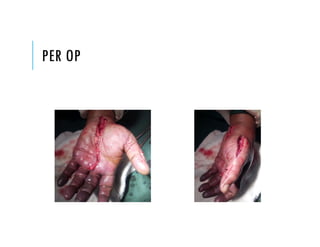
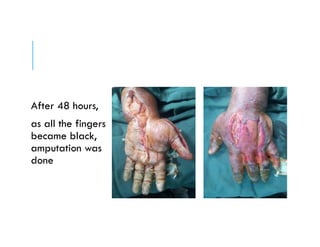
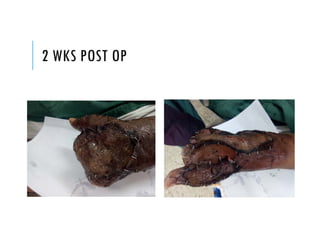
This document discusses a case study of hand infections in diabetic patients. 49 diabetic patients with hand infections were examined. The majority had deep infections involving bone or joints. Many required multiple surgeries and amputations. Poor glucose control and insulin dependence were associated with worse outcomes. Aggressive surgical debridement and antibiotic treatment are needed to manage these infections, which often have severe consequences if not properly treated.