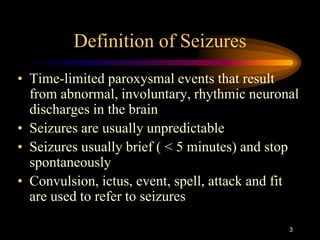
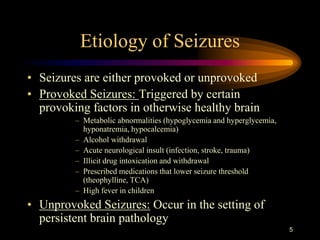
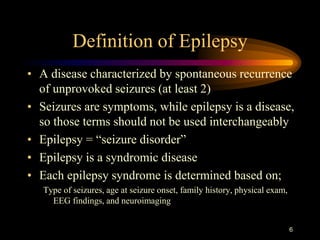
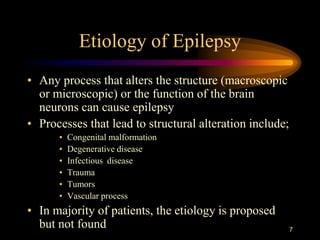
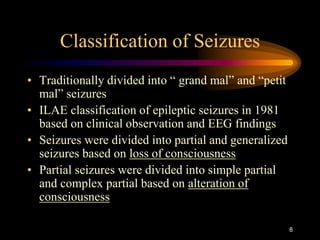
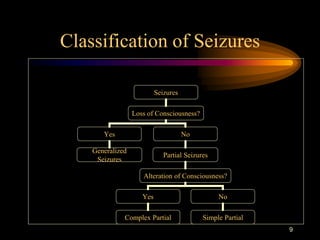
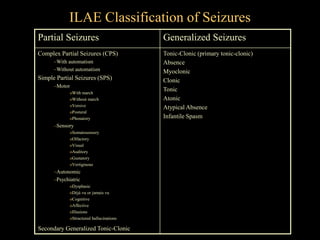
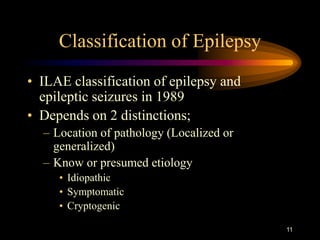
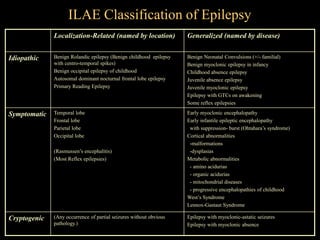
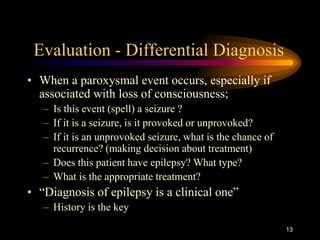
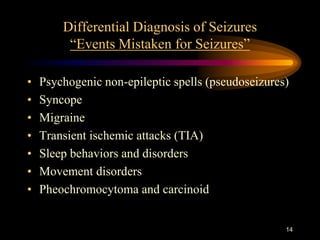
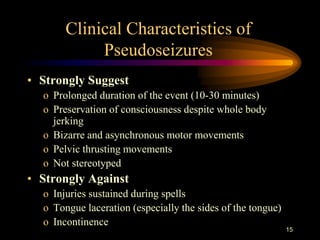
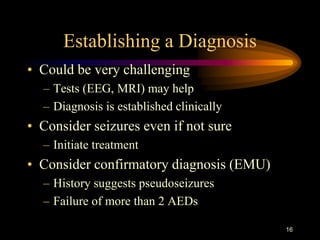
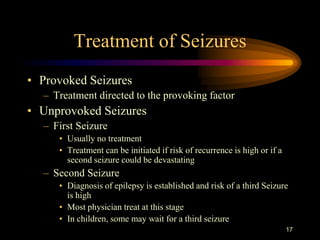
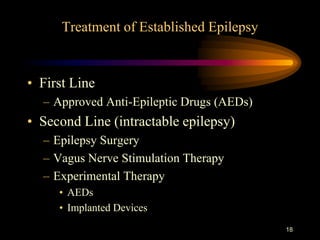
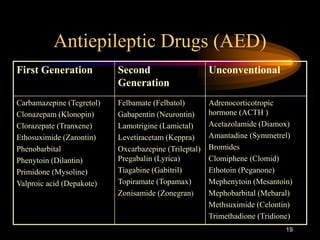
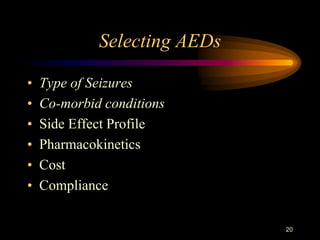
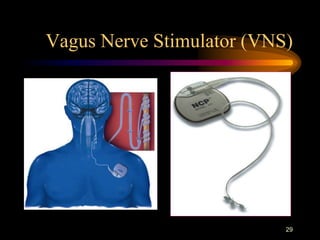
1) The document defines seizures and epilepsy, discusses their etiology and classifications. It also covers evaluating differential diagnoses, treatment options including antiepileptic drugs, epilepsy surgery and vagus nerve stimulation for intractable cases.
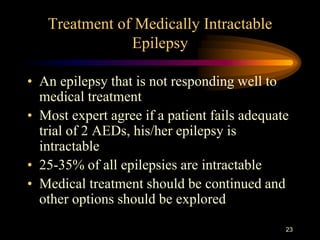
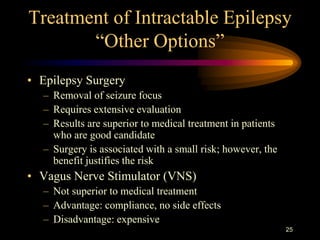
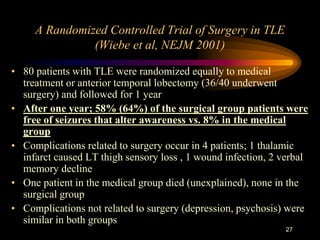
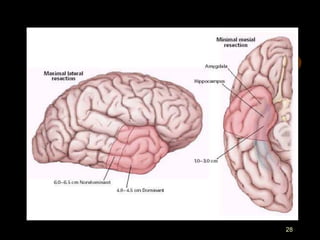
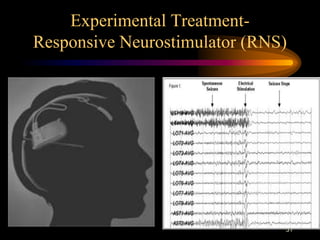
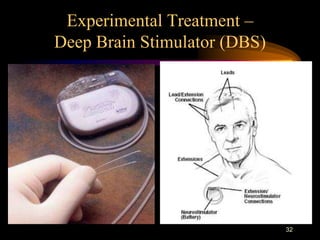
2) Treatment involves using appropriate antiepileptic drugs based on seizure type and side effect profile. For intractable epilepsy, options beyond medical management include epilepsy surgery or vagus nerve stimulation, which have better outcomes than continued drug treatment alone.
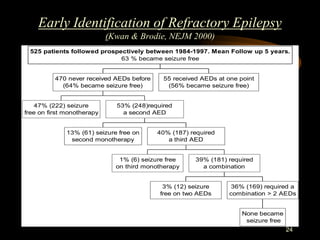
3) The document reviews evidence that early identification of refractory cases allows consideration of alternative treatments, as success rates of additional antiepileptic drugs decline rapidly as treatment fails to control seizures.