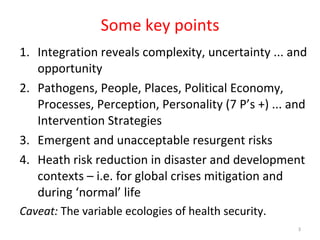
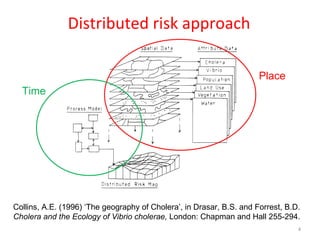
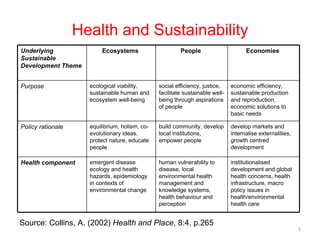
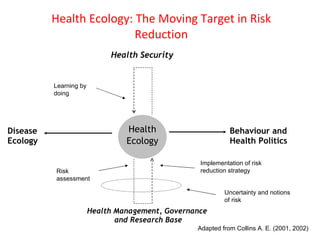
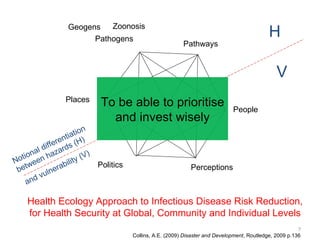
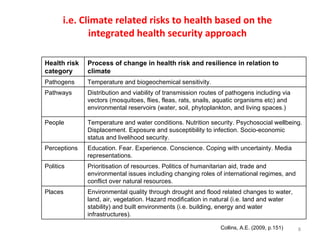
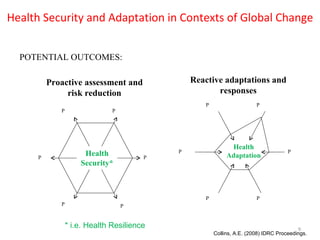
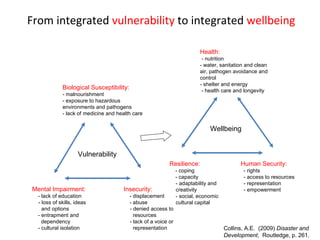
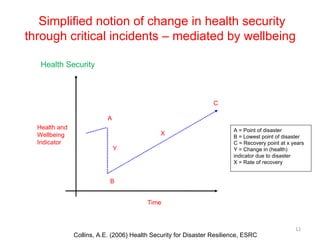
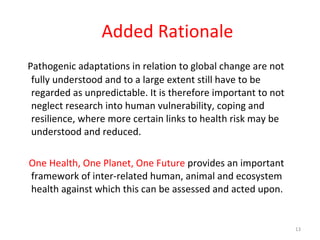
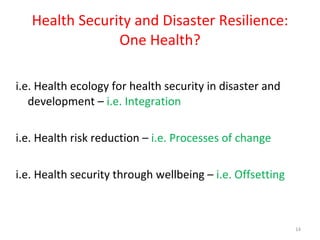
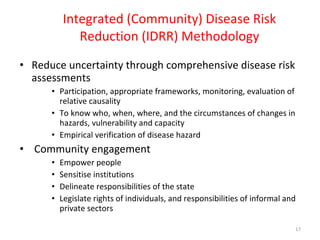
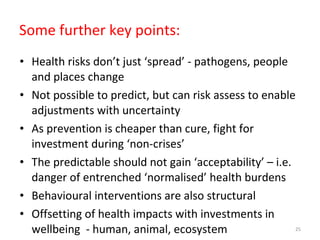
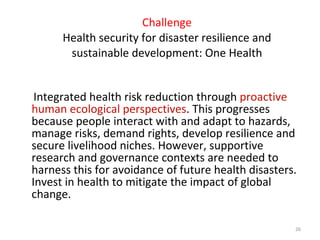
The document discusses integrated health risk management and its relevance in developing areas, highlighting the complexities and opportunities surrounding health security, disease management, and the role of ecological and social contexts in disaster resilience. It emphasizes the need for community engagement and comprehensive assessments to reduce uncertainty in health risks and improve well-being through proactive strategies. The importance of addressing intertwined health, environmental, and socio-economic issues is underscored, advocating for a unified approach to health security and sustainable development.
![Integrated Health Risk Management in Developing Areas GRF One Health Summit 2012 Davos, Switzerland 19 th to 22 nd February, 2012 Andrew Collins Disaster and Development Centre (DDC) Northumbria University, UK [email_address] www.northumbria.ac.uk/ddc](https://image.slidesharecdn.com/andrewcollinsonehealthsummit2012-120222062016-phpapp02/75/Integrated-Health-Risk-Management-in-Developing-Areas-1-2048.jpg)