The document provides information on independent nurse practitioners (INPs) including:
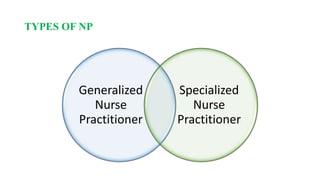
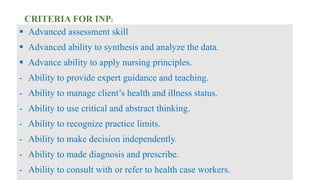
1. It defines INPs as skilled healthcare providers who can perform comprehensive assessments, make diagnoses, and prescribe pharmacological treatments to manage illnesses.
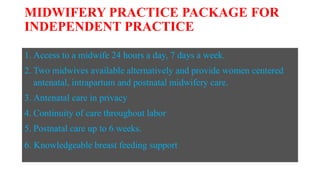
2. The role of INPs originated to increase access to primary care. By the 1990s, many INP programs were developed in response to healthcare reform demands.
3. INPs focus on prevention, wellness, and patient education. They make fewer prescriptions and less expensive treatment while informing and involving patients in their care.
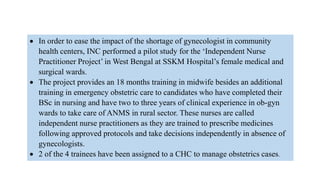
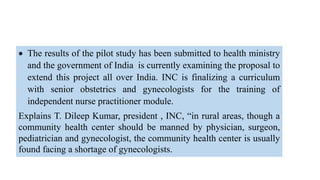
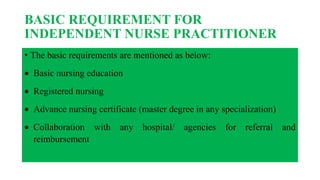
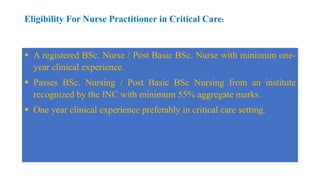
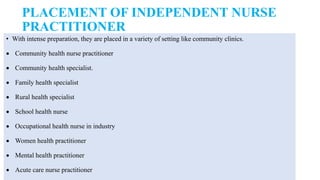
4. INPs must have advanced nursing education, usually a master's degree. They are trained to practice independently or collaboratively in settings like community clinics