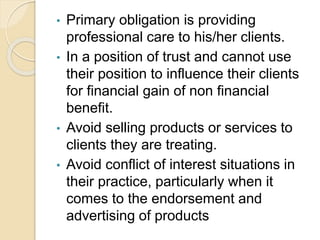
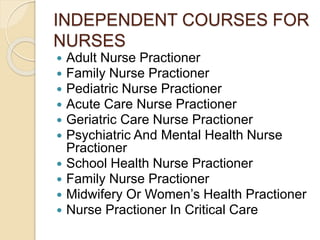
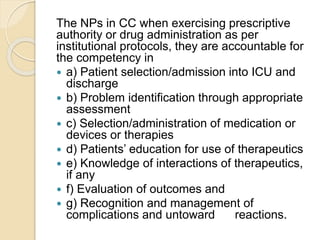
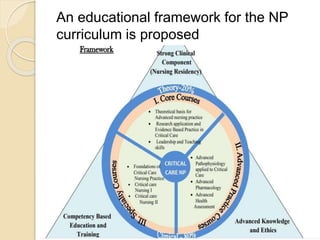
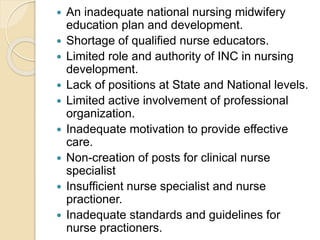
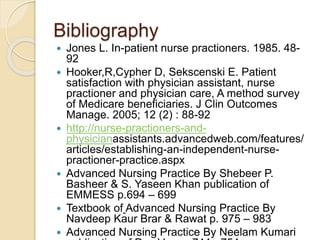
The document discusses independent practice issues for nurses. It defines an independent nurse practitioner as an advanced practice nurse with a master's degree in a specialized area who is licensed to practice independently in their state. The seminar objectives are to define an independent nurse practitioner, list courses available, and analyze issues they may face. The document outlines the philosophy, historical development, key practices, educational requirements, responsibilities and issues of independent nurse practitioners. It also discusses the process nurses go through from novice to expert and lists some independent courses available for nurses.