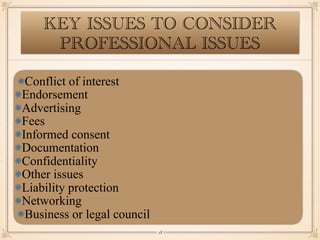
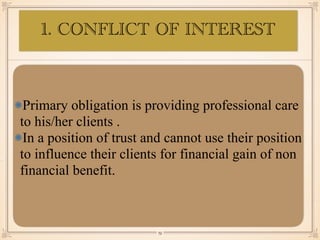
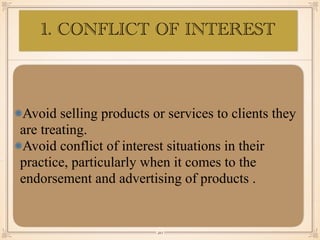
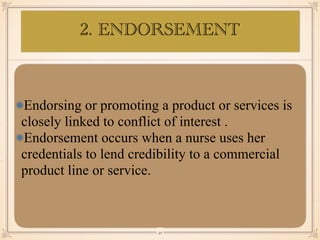
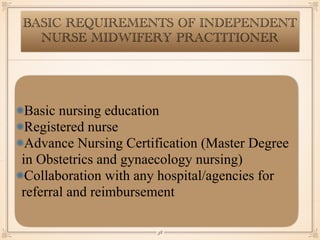
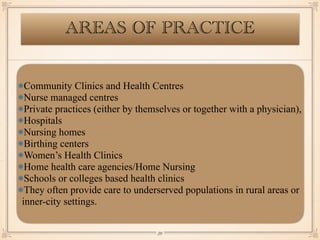
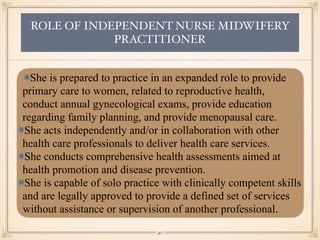
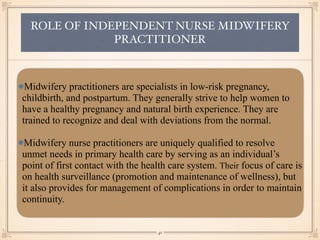
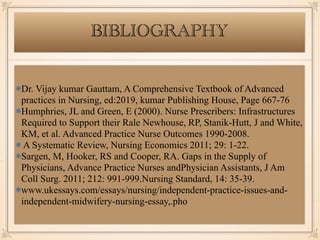
The document discusses independent nurse practitioners, specifically independent nurse midwifery practitioners. It defines independent nurse practitioners as advanced practice nurses with a master's degree who are licensed to practice independently. It outlines the philosophy, historical development, standards, key practices, and issues of independent midwifery practice. It also discusses the development of independent nurse practitioners in India to address shortages and reduce maternal and infant mortality rates.