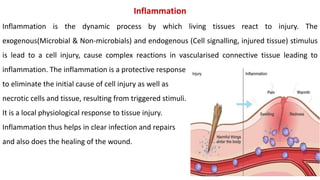
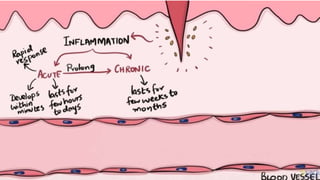
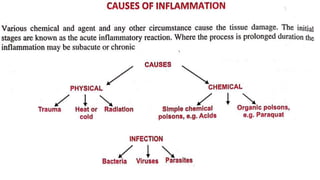
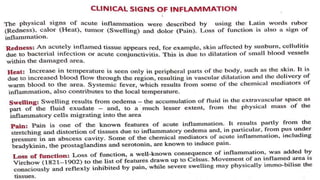
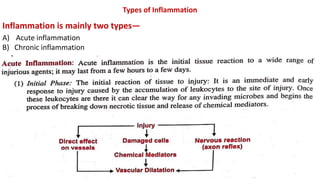
The document provides a detailed overview of inflammation and its types, highlighting acute and chronic inflammation, along with the processes involved in each. It discusses the cellular events, vascular changes, mediators of inflammation, and the basic principles of wound healing through primary and secondary union. Additionally, it outlines potential complications during the healing process, such as infections and deficient scar formation.