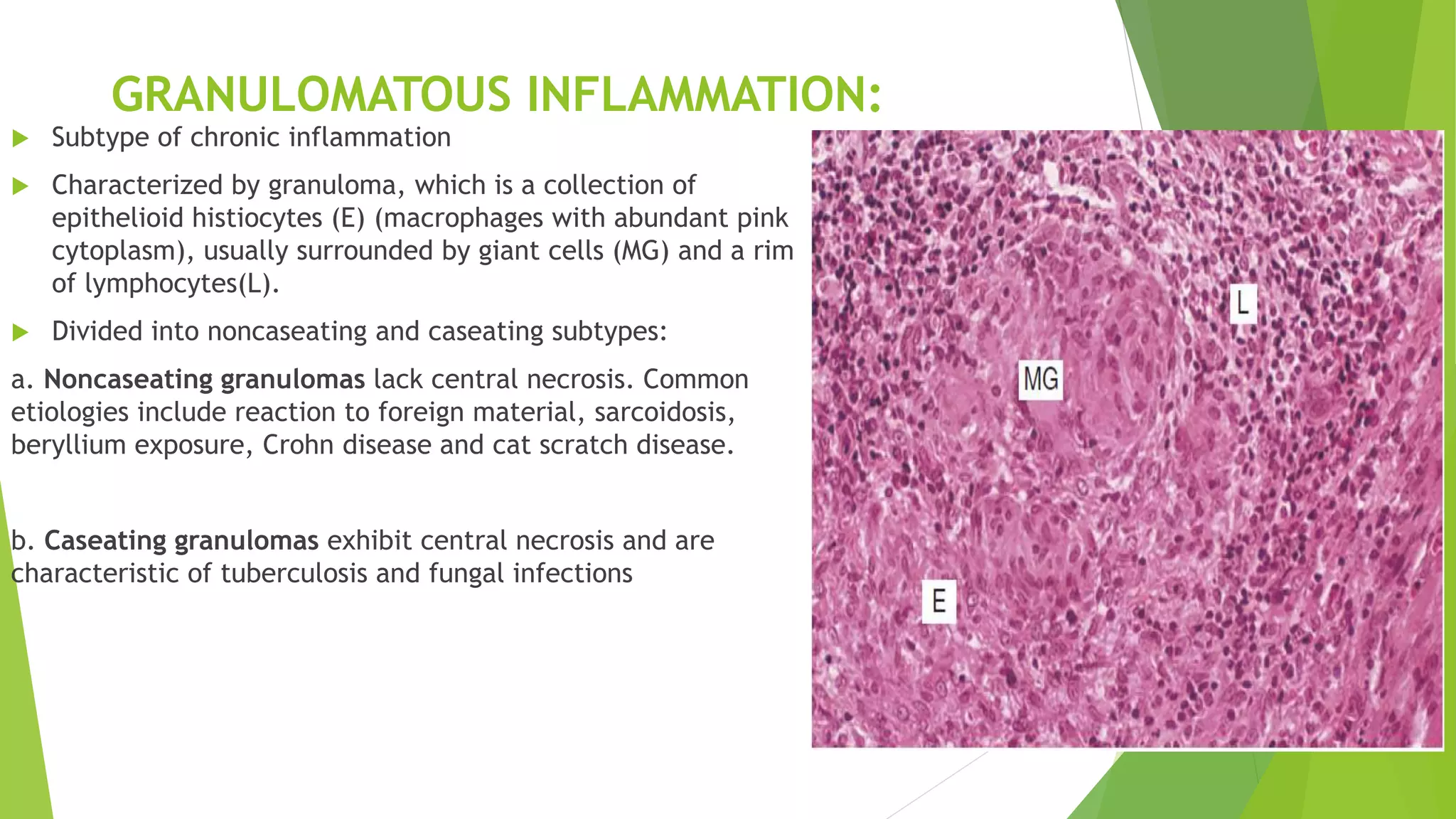
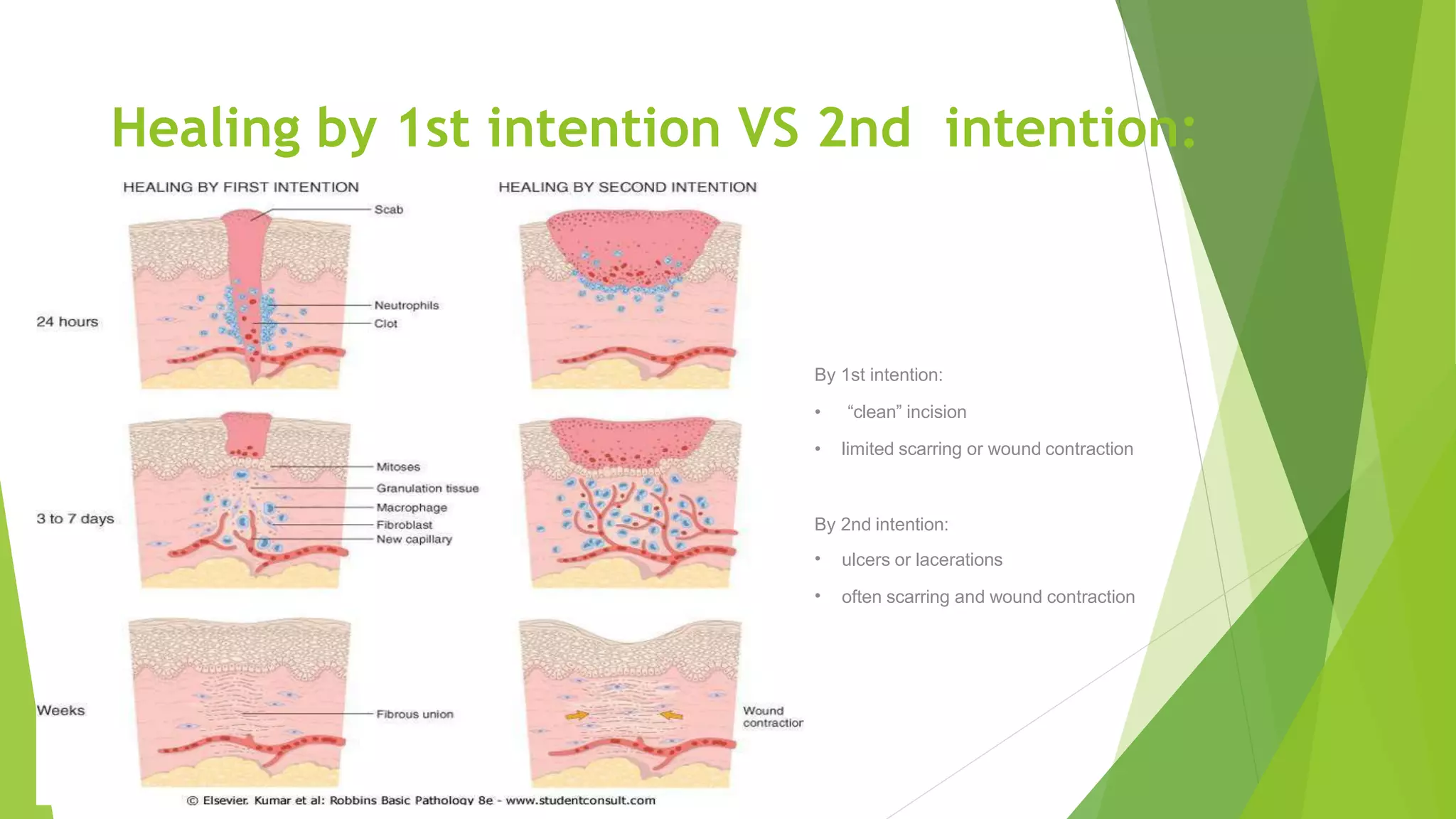
This document discusses acute and chronic inflammation and wound healing. It defines inflammation and describes its purpose. There are two main types: acute and chronic inflammation. Acute inflammation is short-term and involves chemicals like toll-like receptors and arachidonic acid metabolites. Chronic inflammation is long-lasting and characterized by lymphocytes and macrophages. It can lead to outcomes like scarring, amyloidosis, or neoplastic transformation. Wound healing involves regeneration or repair through granulation tissue formation and is affected by factors like infection, nutrition, and vascular disease. Abnormal wound healing can result in dehiscence or scarring.



![Acute Inflammation:
Acute inflammation is a transient and early response to injury that is
characterized by the release of numerous chemical mediators and leads to
stereotypic small vessel and leukocyte (white blood cell [WBC]) responses.](https://image.slidesharecdn.com/acuteandchronicinflammationwoundhealing-200909193702/75/Acute-and-Chronic-inflammation-Wound-Healing-4-2048.jpg)