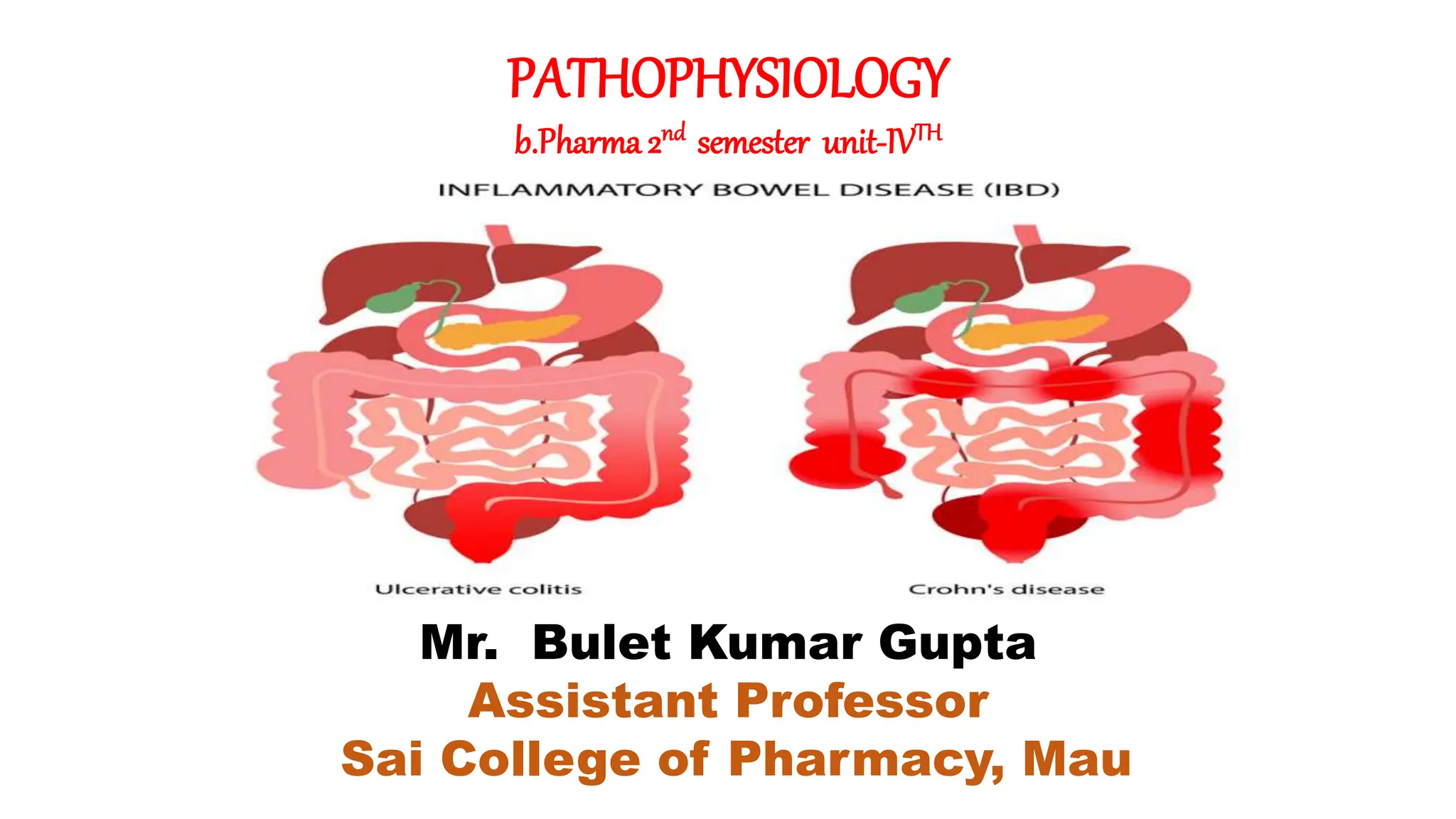
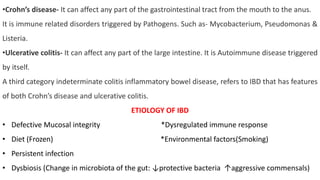
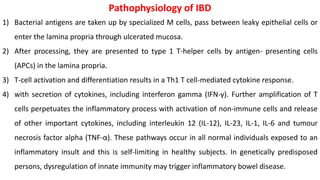
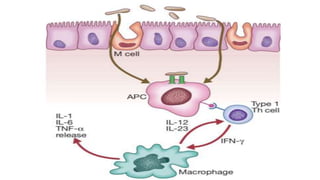
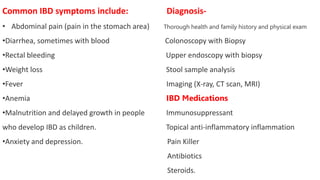
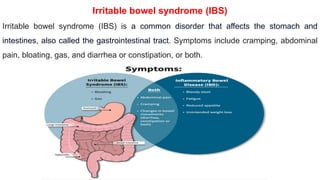
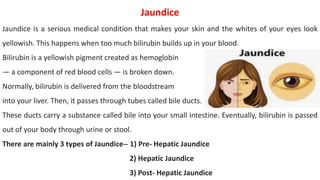
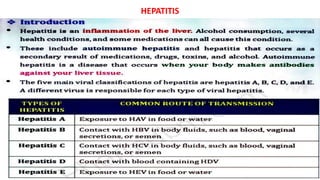
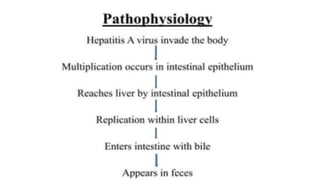
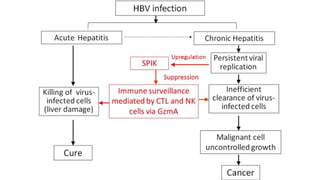
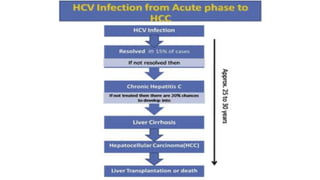
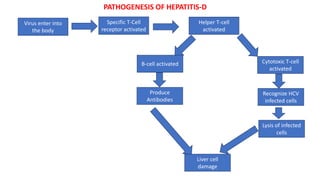
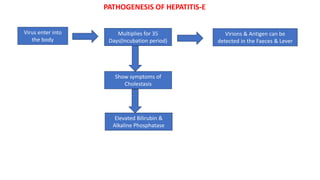
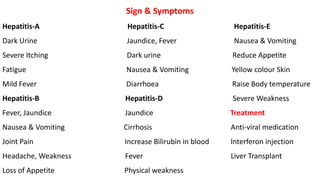
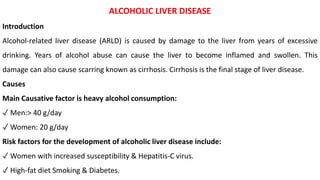
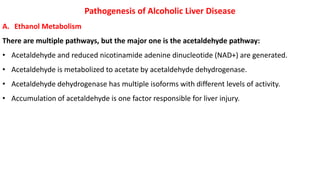
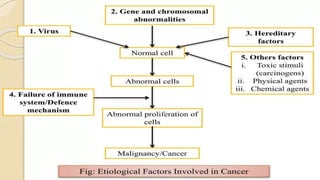
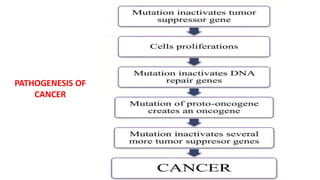
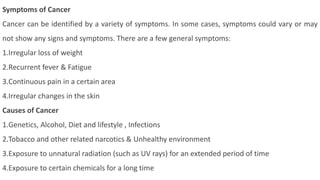
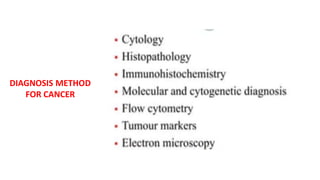
The document discusses various medical conditions, focusing on inflammatory bowel disease (IBD), hepatitis, and cancer, along with their pathophysiology, symptoms, and diagnostic methods. IBD includes ulcerative colitis and Crohn's disease, characterized by intestinal inflammation, while hepatitis involves liver damage due to viral infections. Cancer is classified into types such as carcinoma, sarcoma, leukemia, lymphoma, melanoma, and myeloma, with symptoms that may include weight loss, fatigue, and pain.