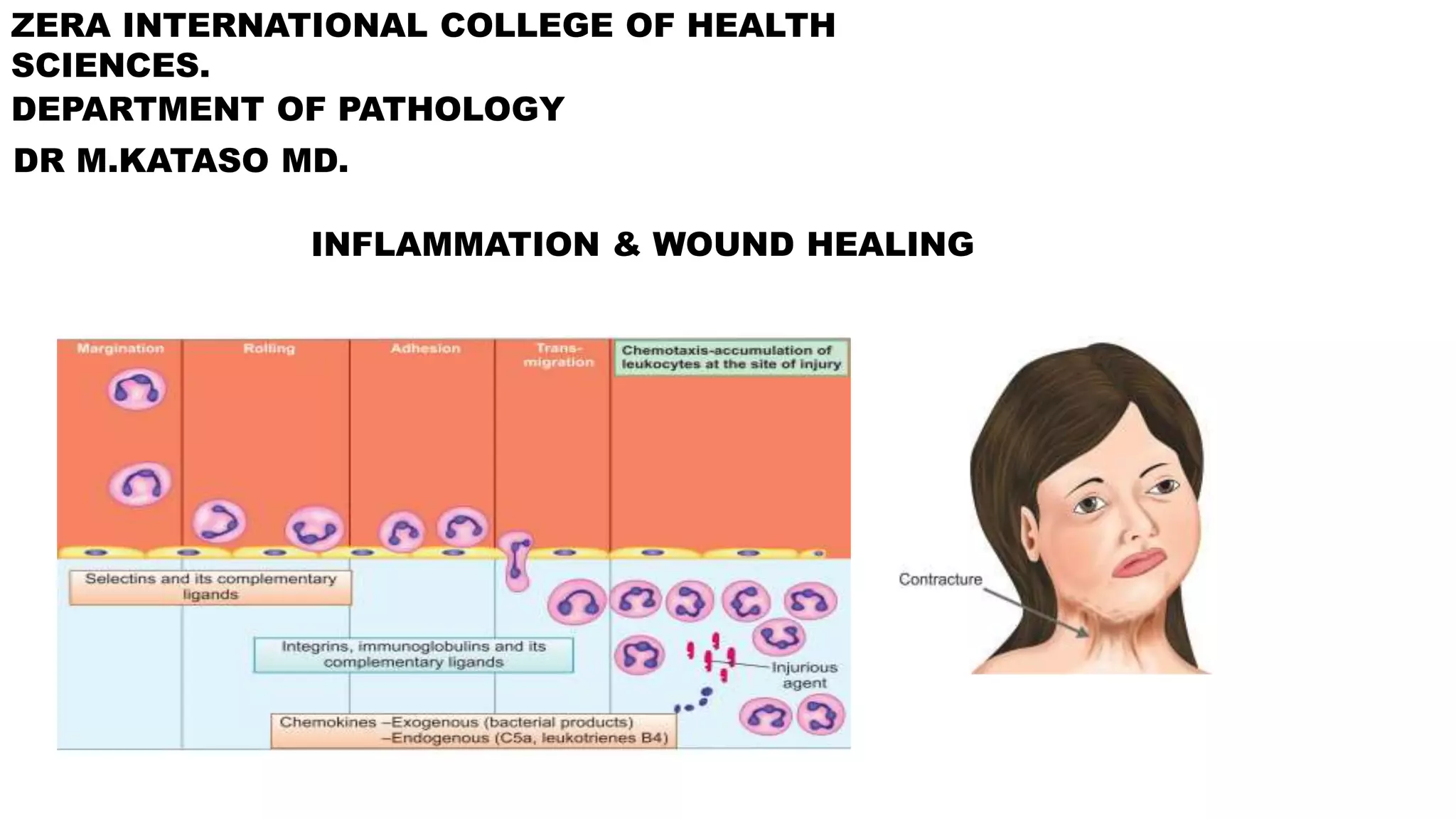
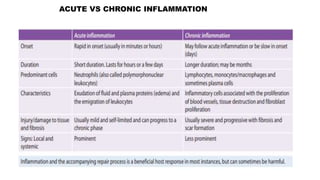
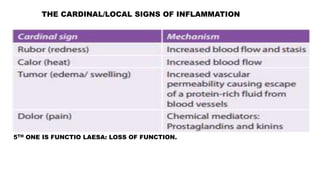
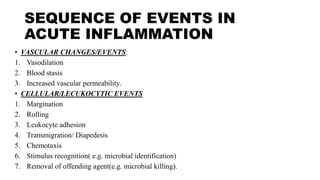
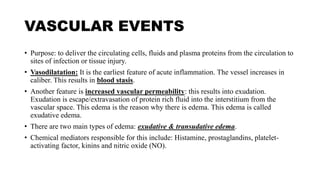
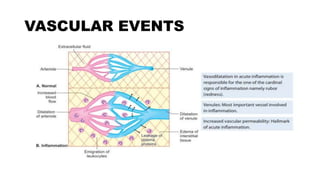
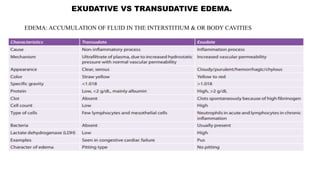
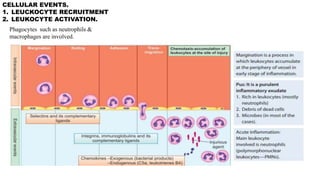
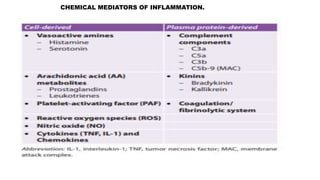
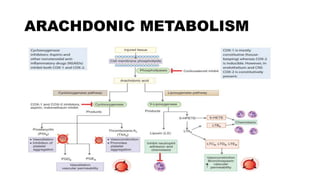
This document discusses inflammation and wound healing. It begins by defining inflammation and describing the cardinal signs. It then discusses the causes and types of inflammation. The sequence of events in acute inflammation is explained, including vascular changes like vasodilation and increased permeability, and cellular events like leukocyte recruitment and activation. Chemical mediators are also discussed. Outcomes of acute inflammation and systemic signs are summarized. Finally, the document covers factors influencing wound healing, the process of cutaneous wound healing, and potential complications.