This document discusses open fractures, including their definition, classification, epidemiology, microbiology, treatment principles, and management. Some key points:
- Open fractures involve a break in the skin and soft tissue leading directly to the fracture site. They were historically associated with high infection and mortality rates.
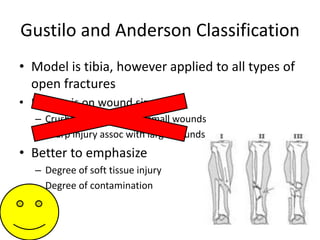
- The Gustilo-Anderson classification system grades open fractures based on the degree of soft tissue injury from I to III (A, B, C). Higher grades correlate with increased risk of infection and impaired fracture healing.
- Most open fracture infections are caused by bacteria acquired in the hospital rather than the initial trauma. Appropriate antibiotic treatment is crucial.
- Goals of management include preserving life and limb,