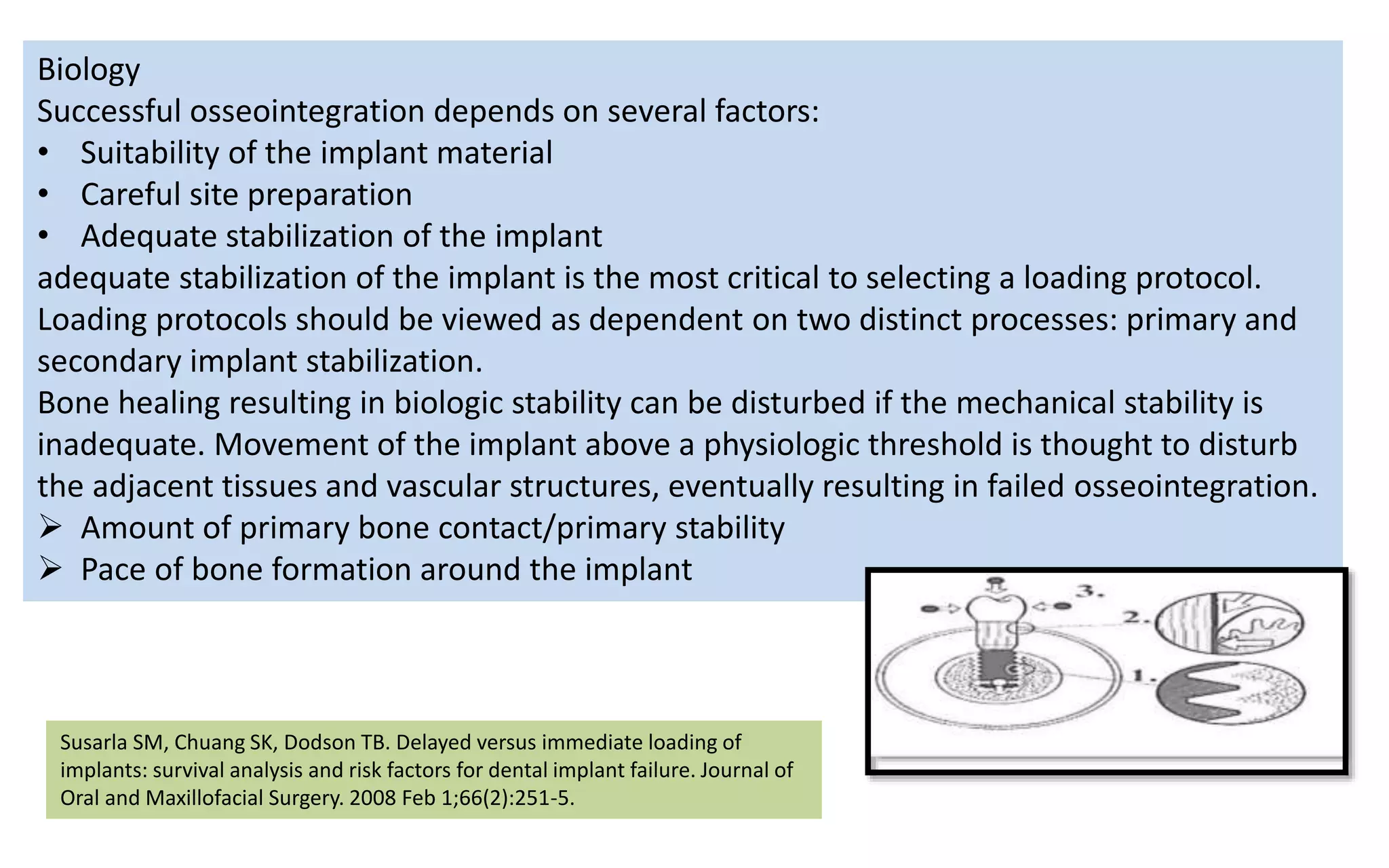
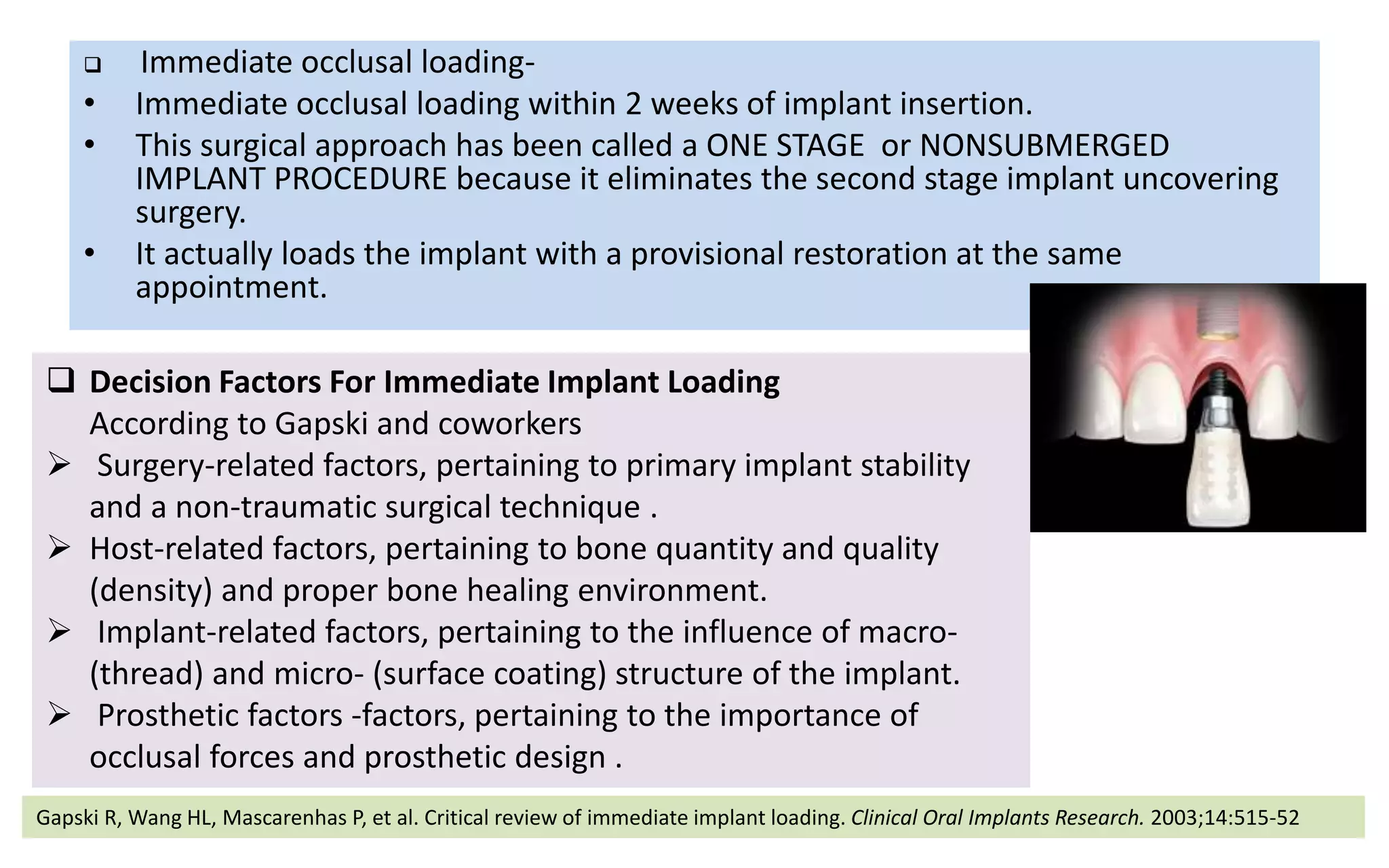
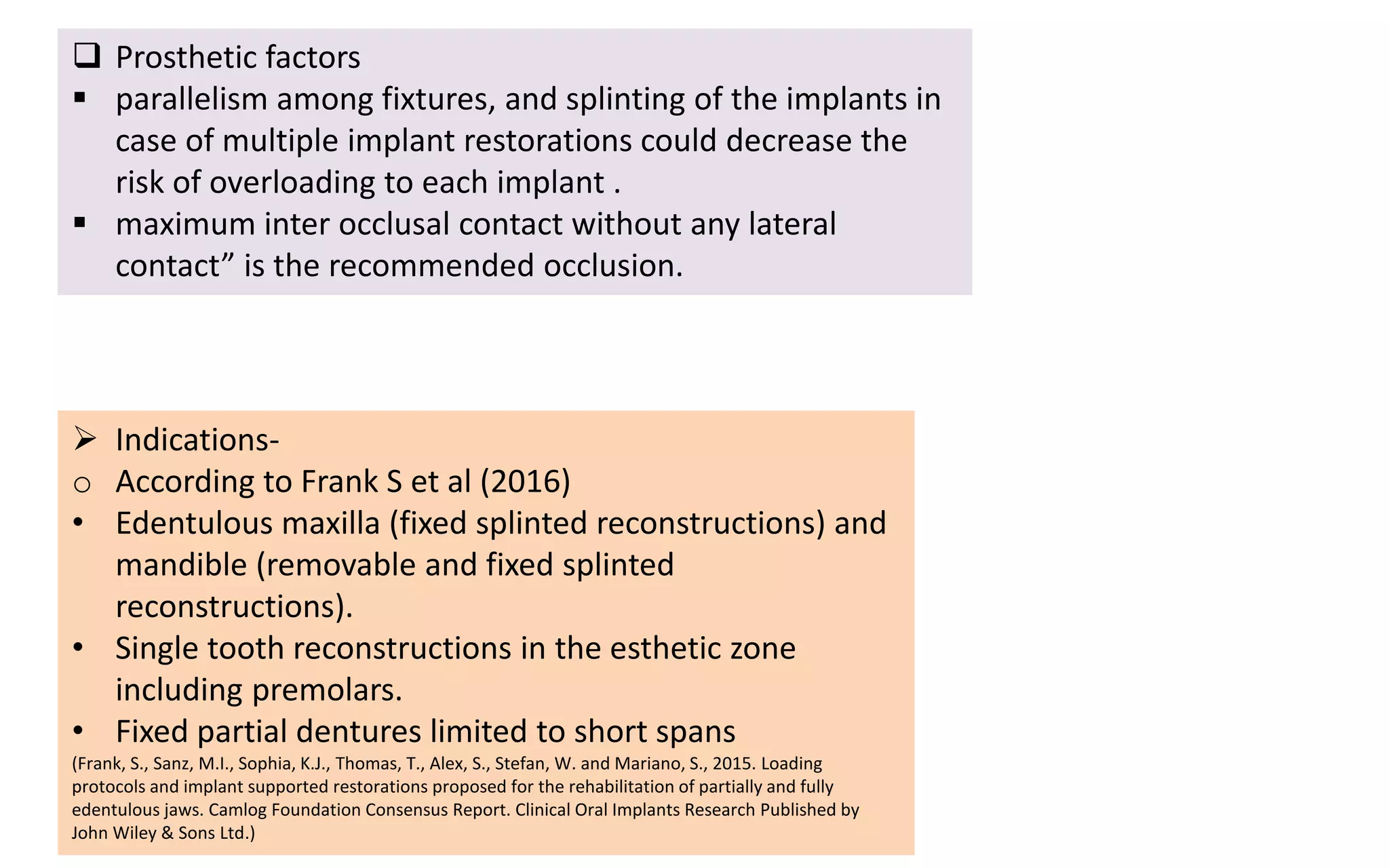
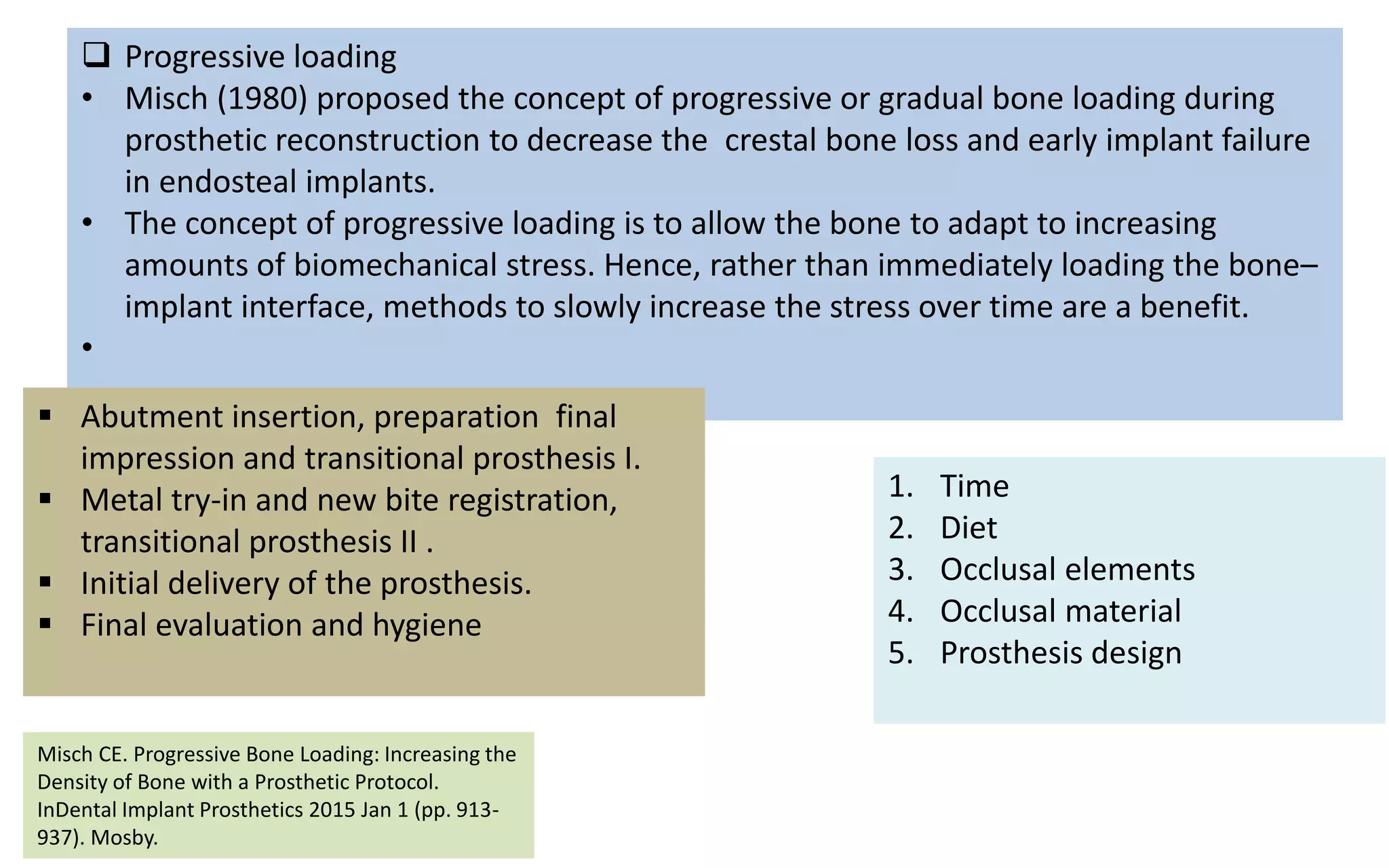
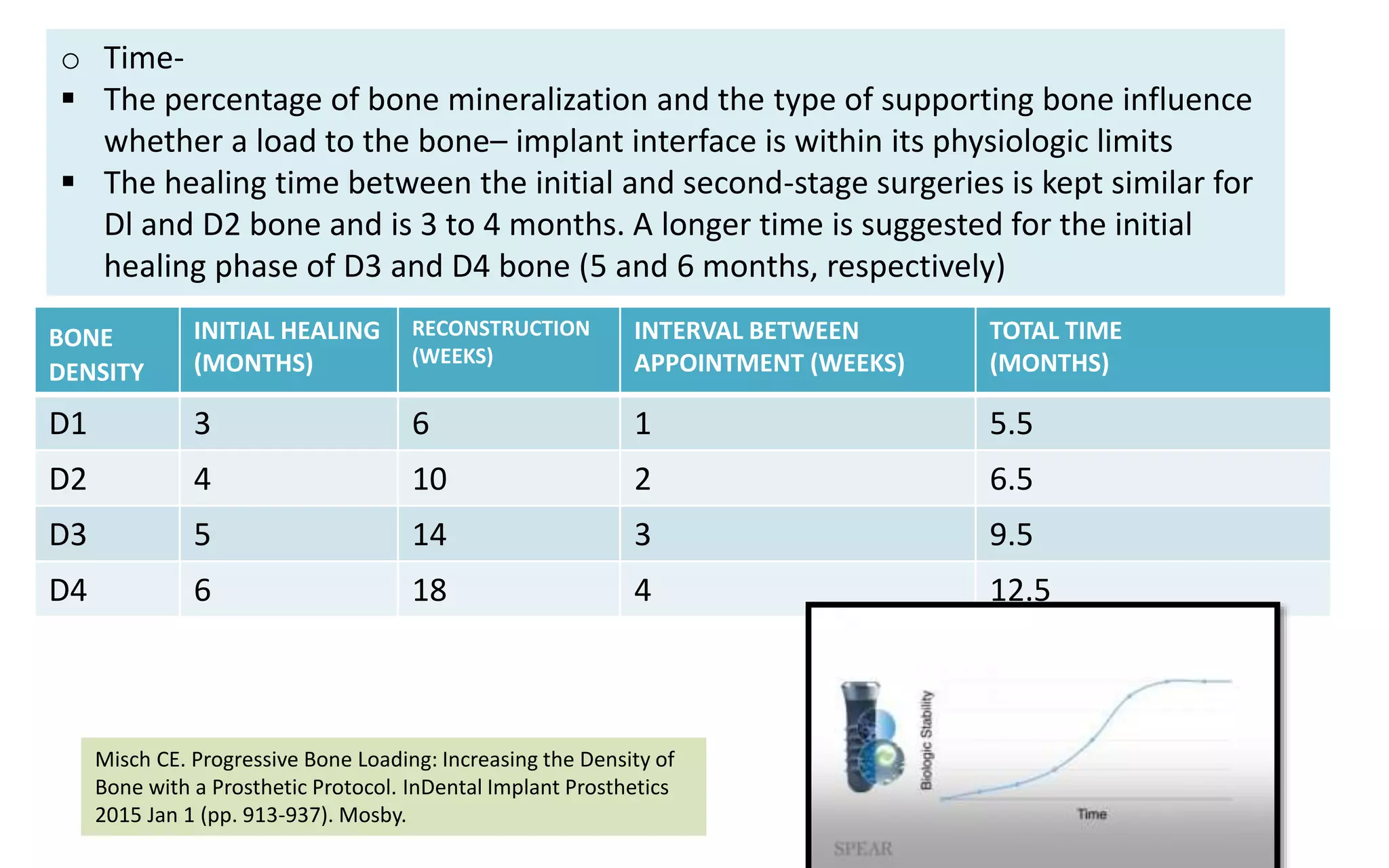
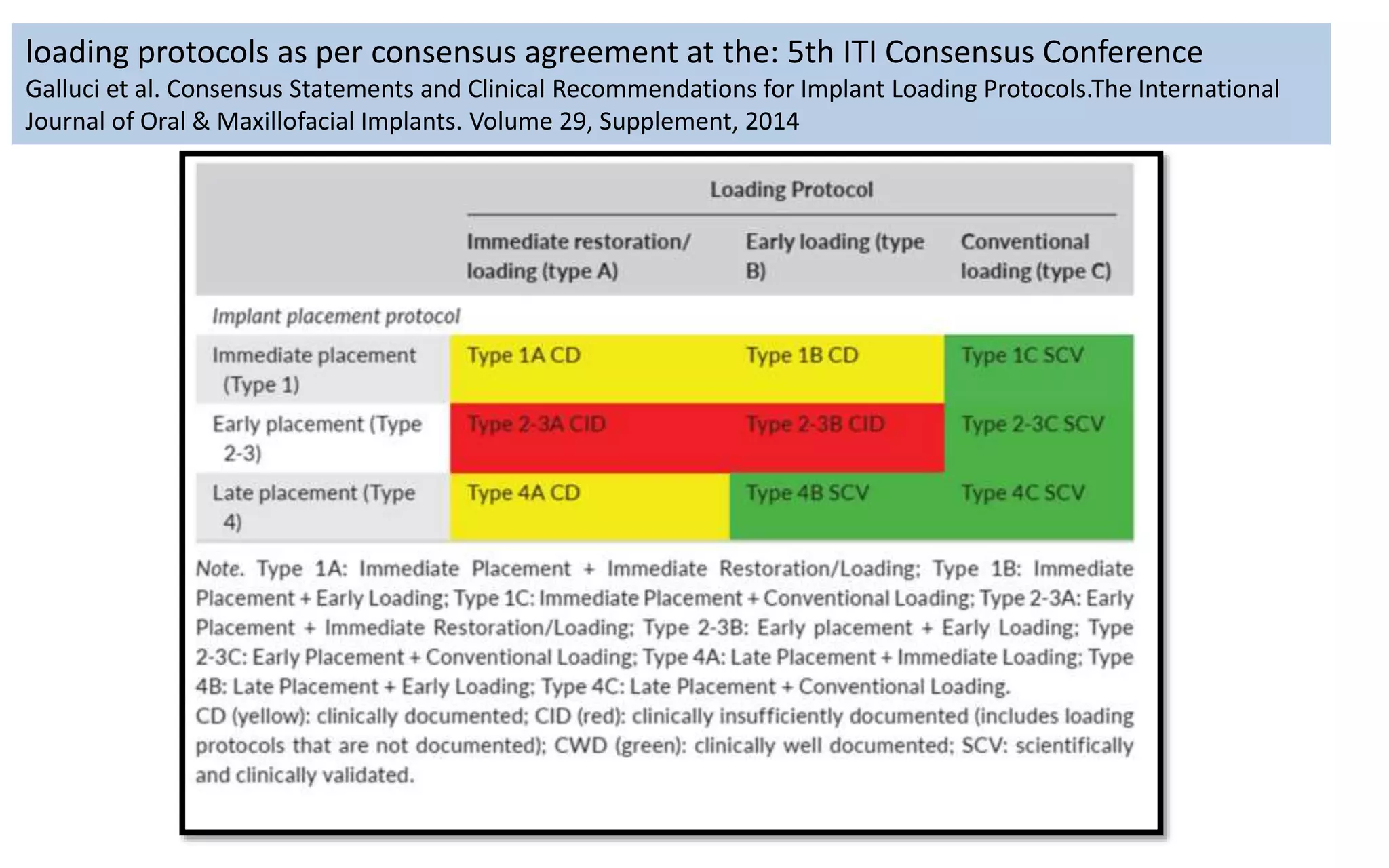
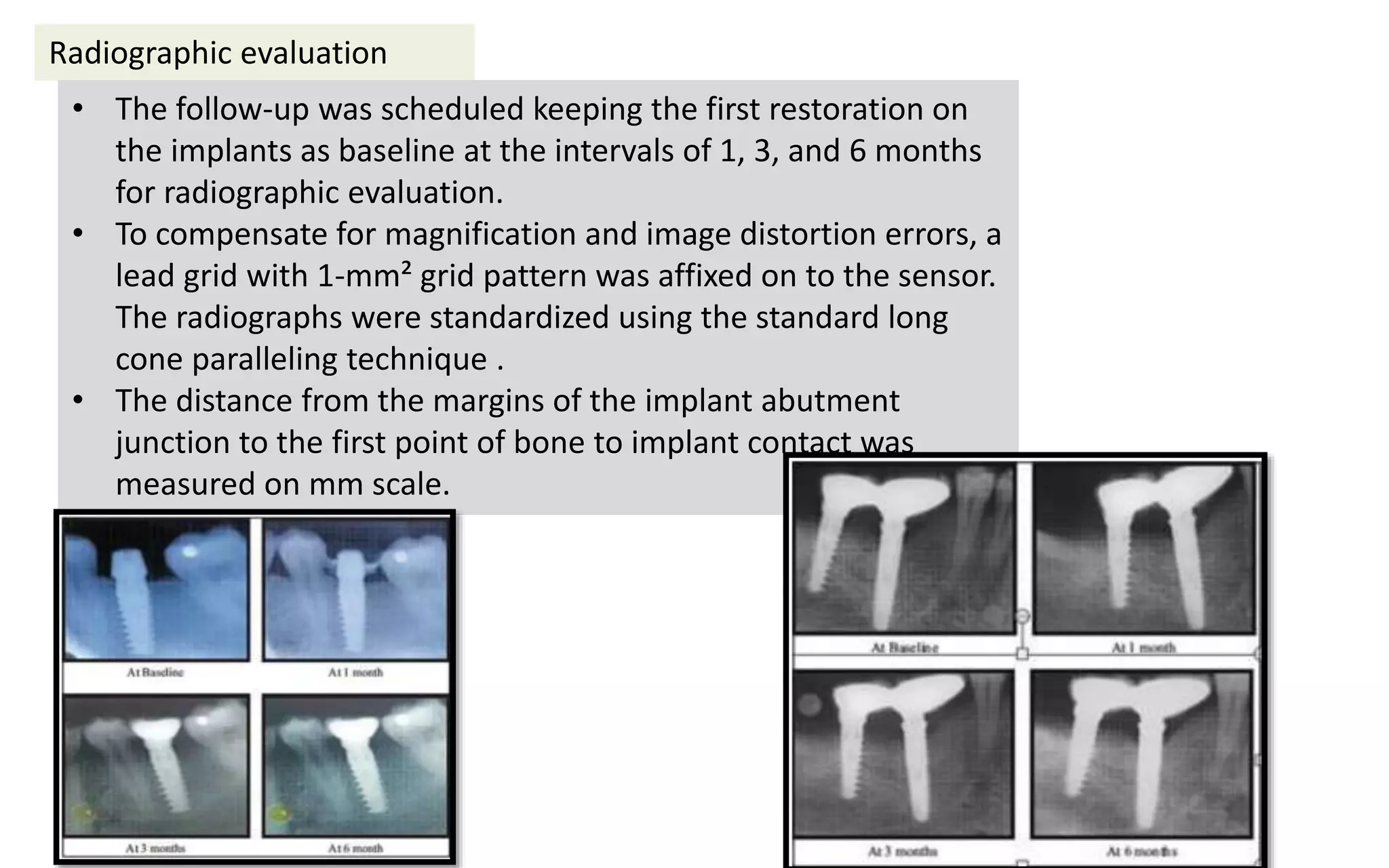
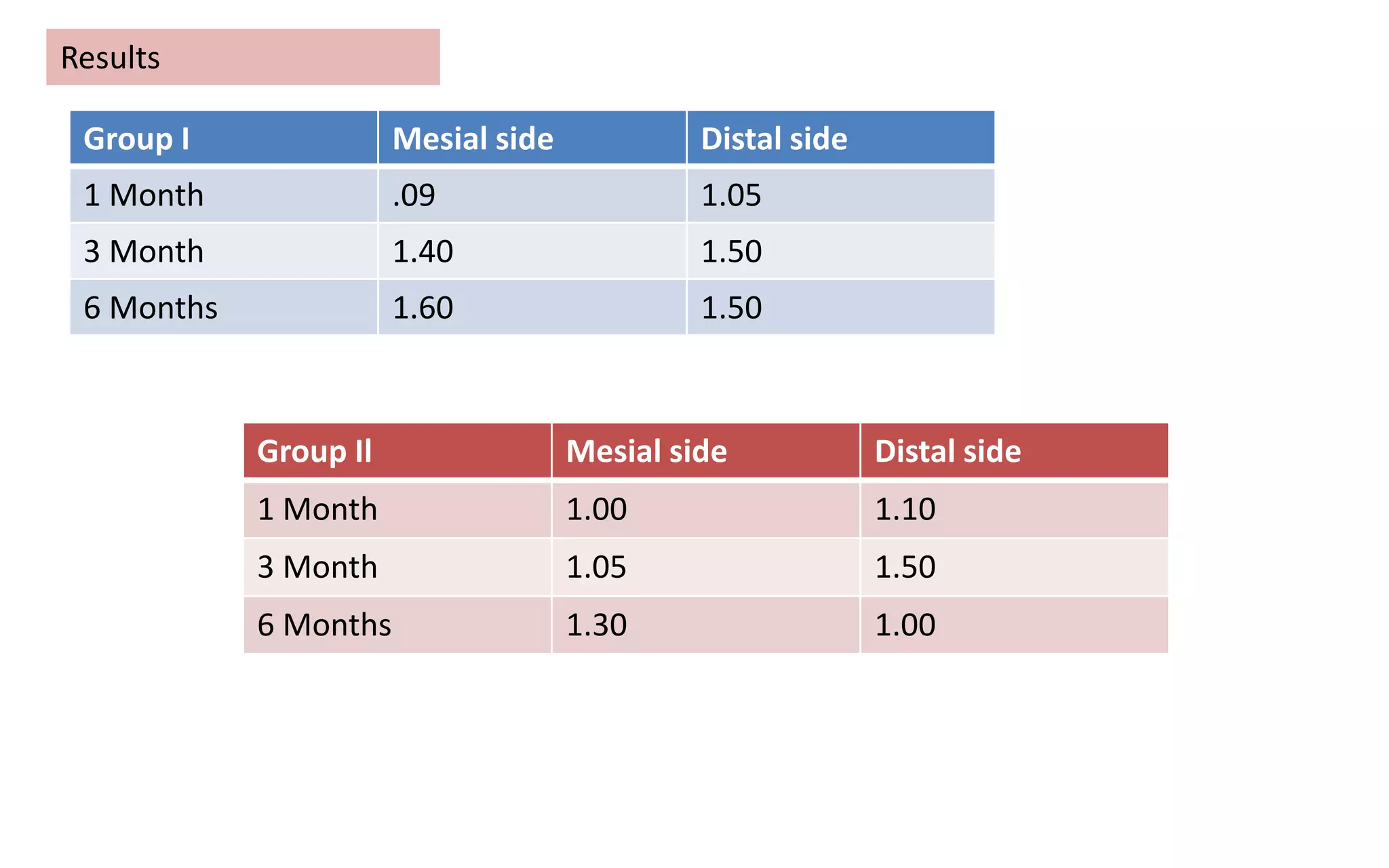
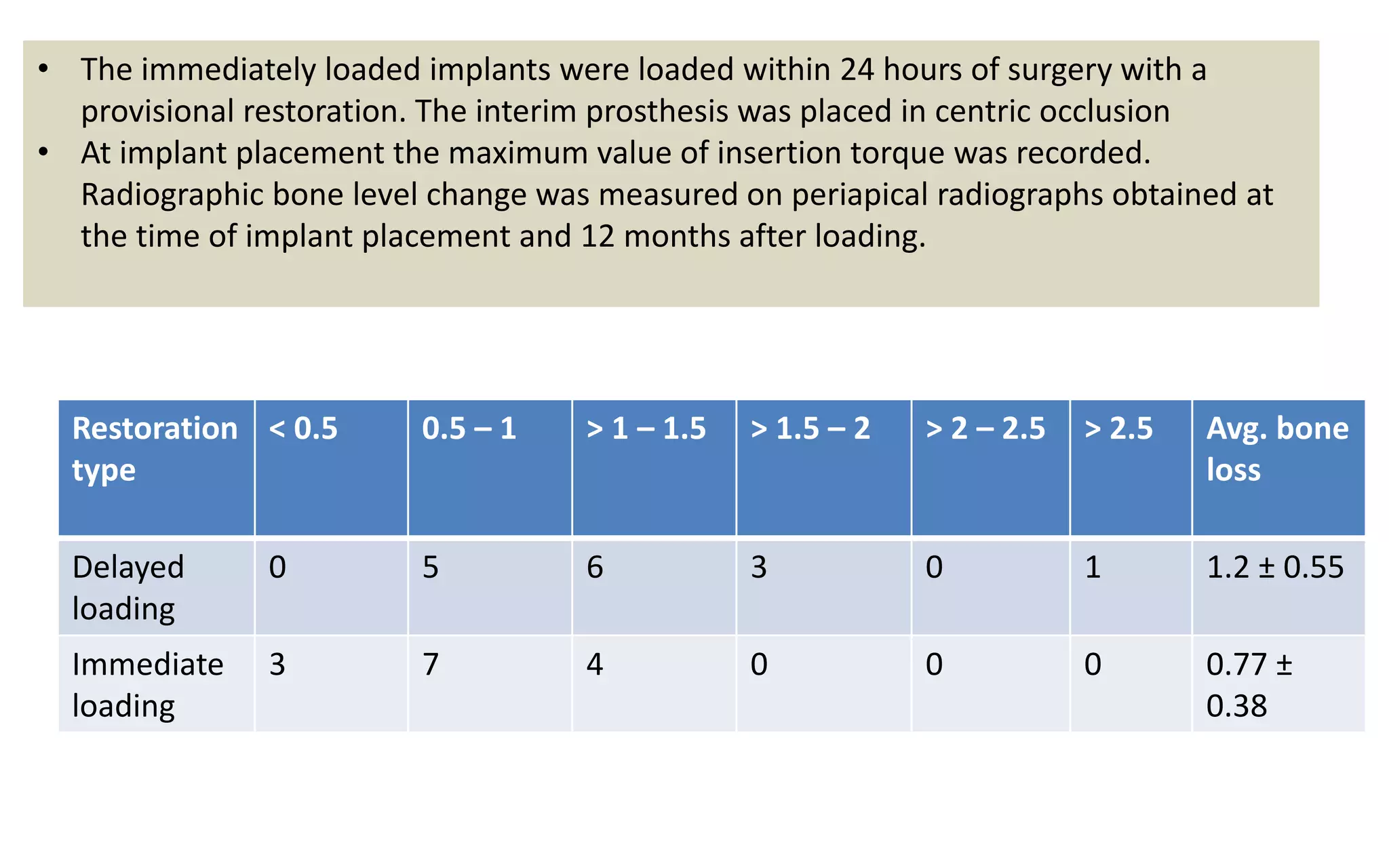
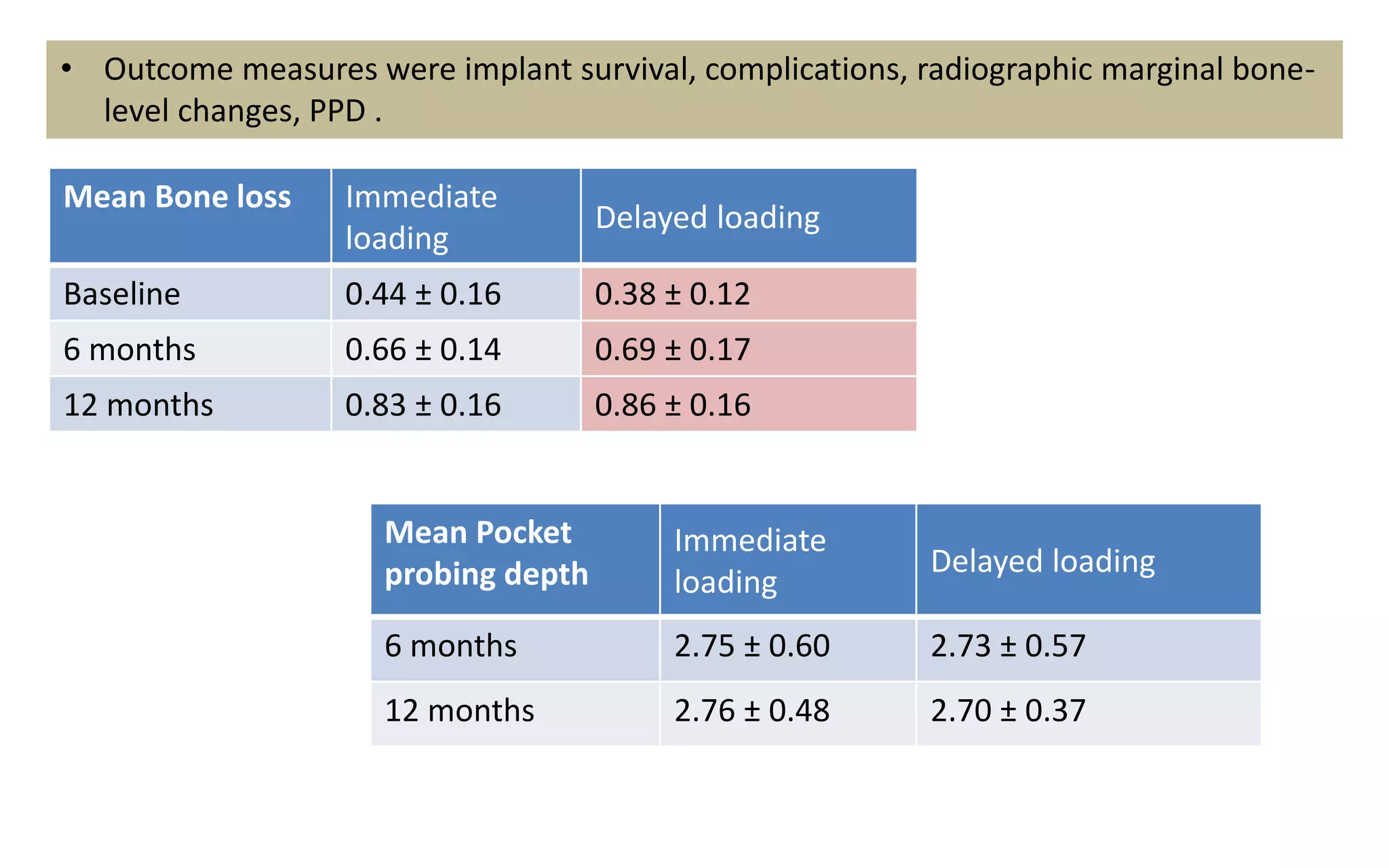
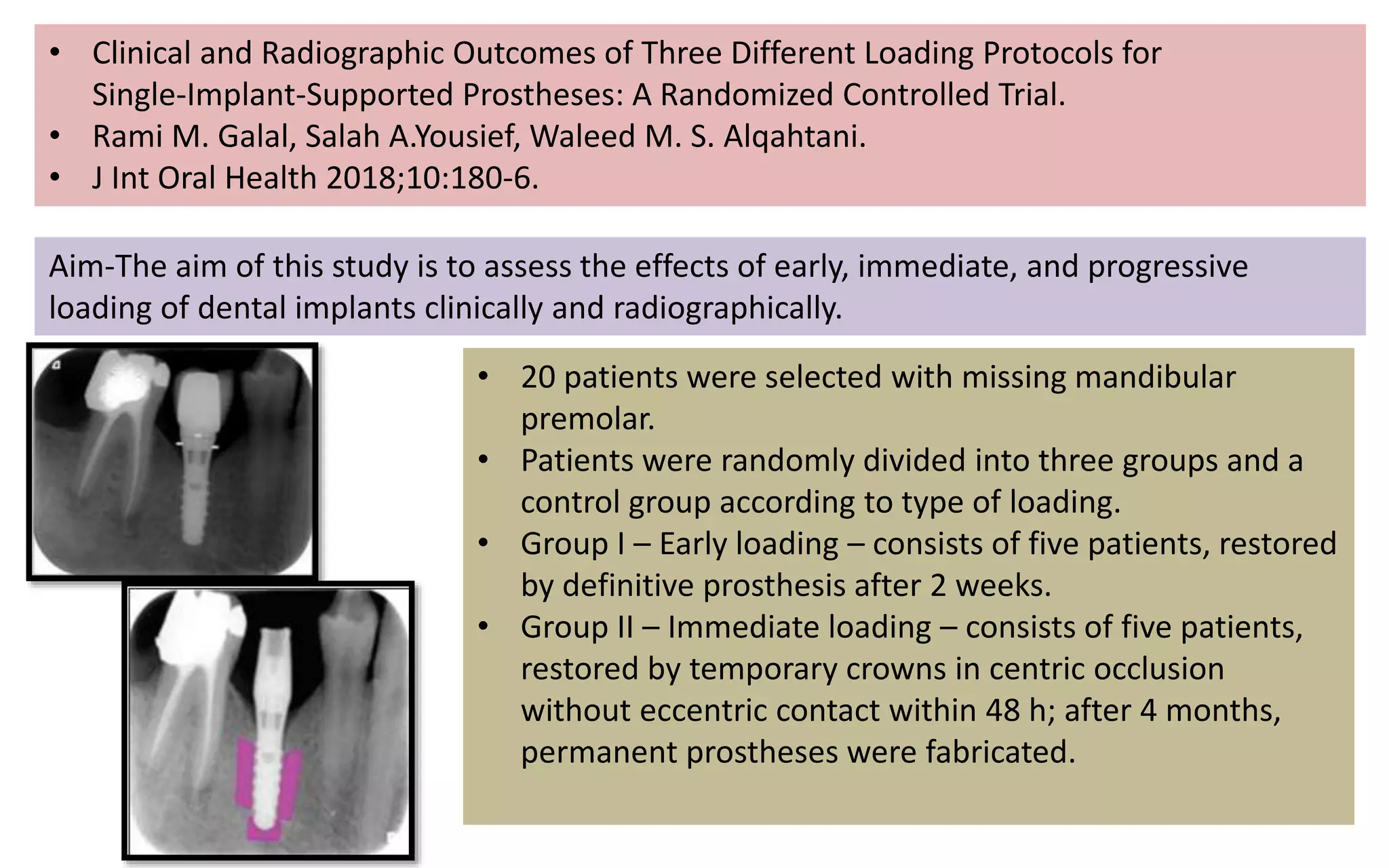
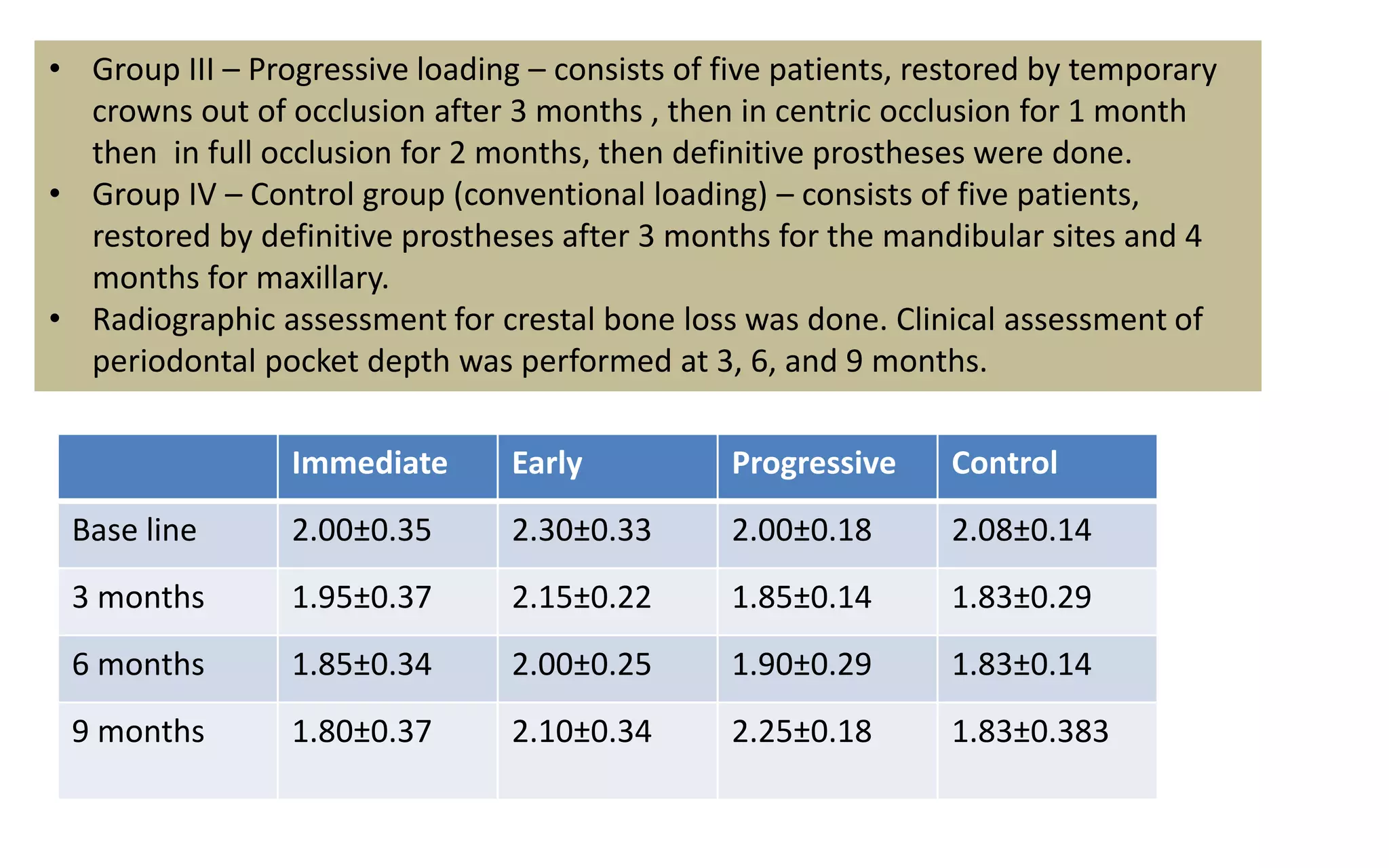
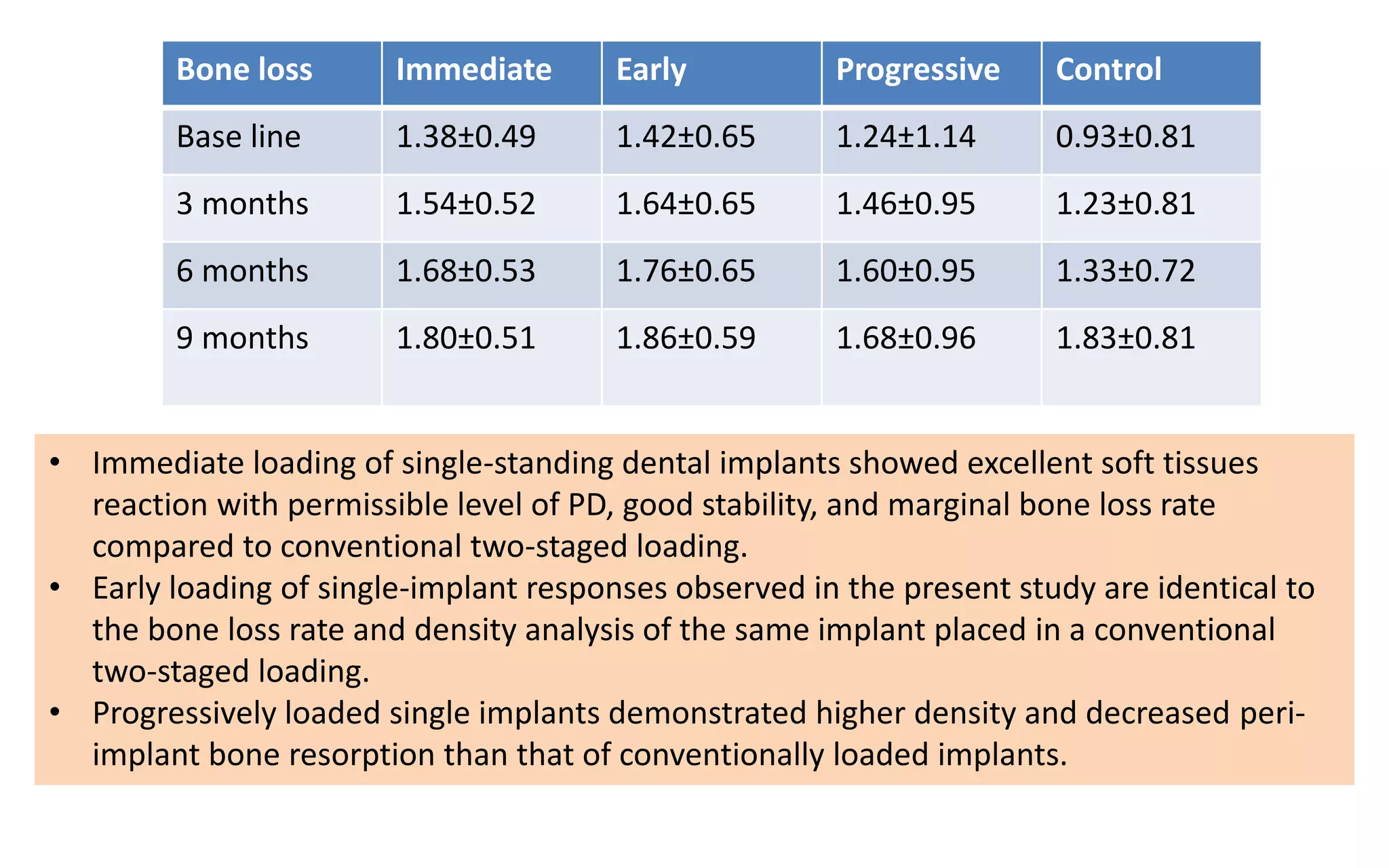
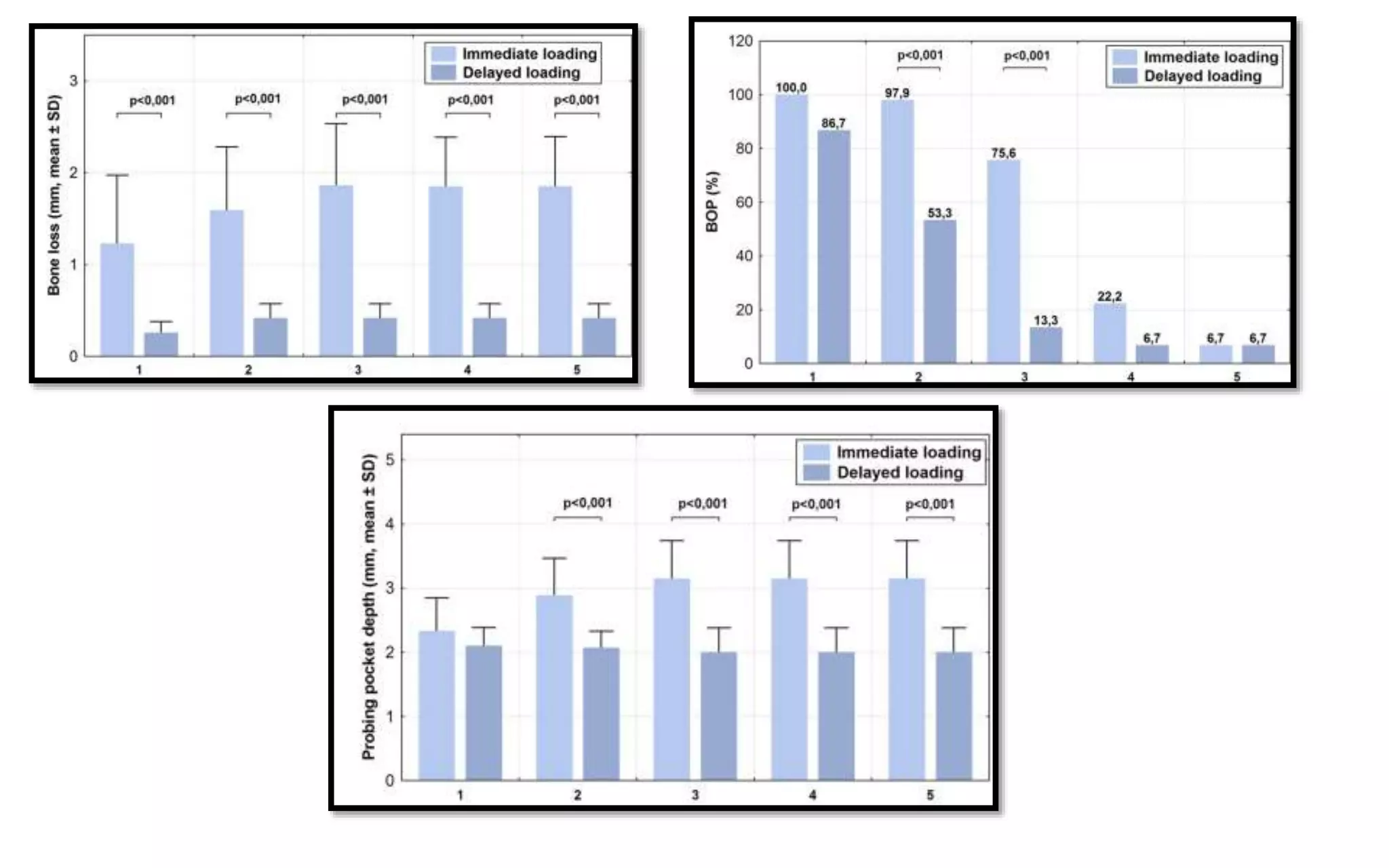
The document presents a comparative study on immediate versus delayed loading protocols of dental implants, highlighting factors affecting osseointegration and clinical outcomes. It discusses different loading conditions and their implications on bone loss and healing, concluding no statistically significant difference in crestal bone loss between the two methods. The study emphasizes the importance of implant stability and individual patient factors in determining the appropriate loading protocol.