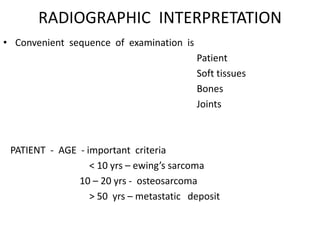
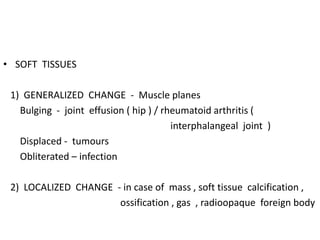
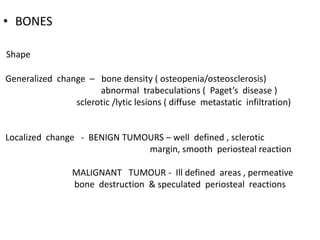
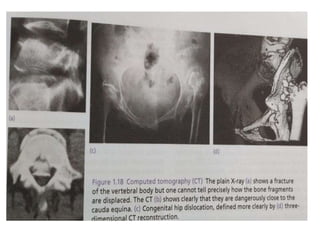
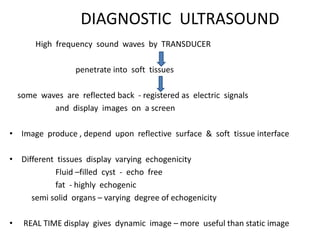
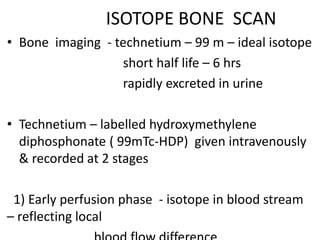
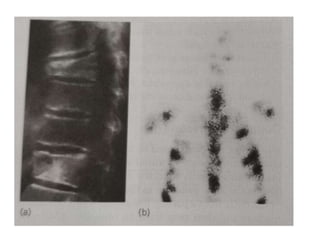
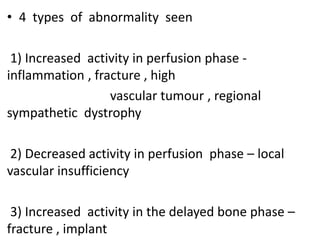
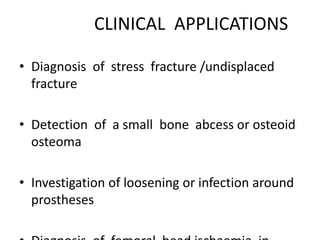
This document provides an overview of various imaging techniques used in orthopaedics, including their principles, applications, advantages, and limitations. It discusses plain film radiography, computed tomography, magnetic resonance imaging, ultrasound, radionuclide imaging techniques like bone scintigraphy, and emerging techniques like SPECT and PET imaging. The key information provided includes the physical principles behind each technique, their clinical utility in evaluating bone fractures, tumors, infections and other musculoskeletal abnormalities, and factors like radiation exposure, soft tissue contrast, and cost.