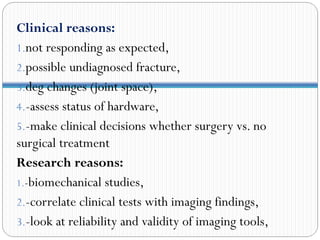
Diagnostic imaging modalities play an important role in physical therapy. Rehab doctors need to understand medical imaging to make informed treatment decisions and assess patient progress or complications. The summary discusses several common imaging modalities:
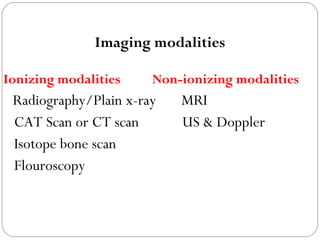
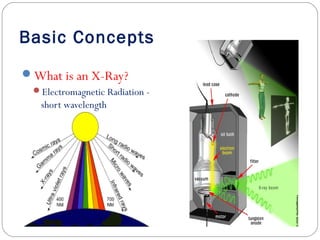
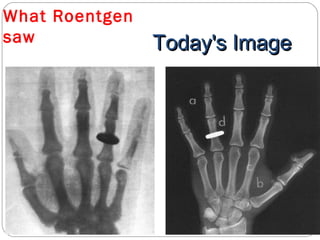
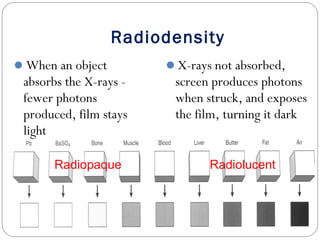
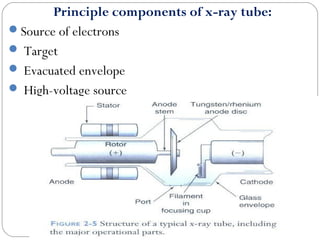
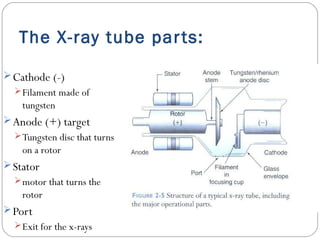
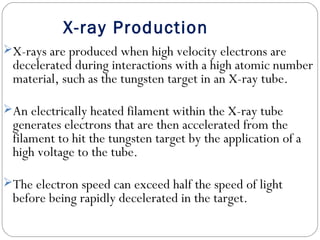
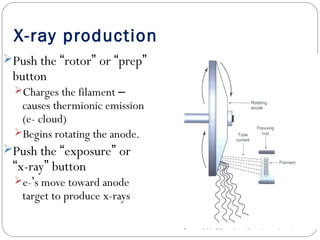
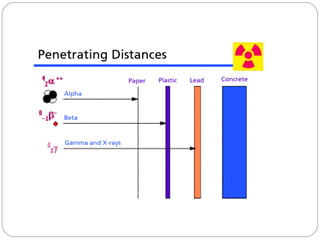
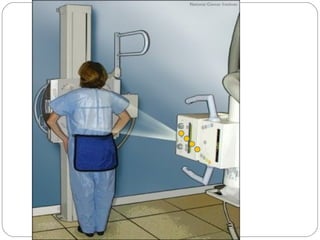
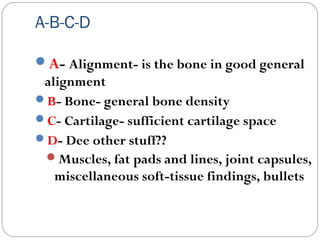
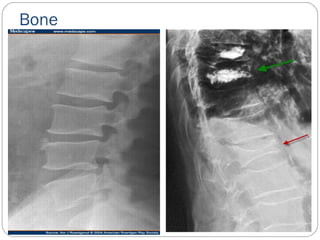
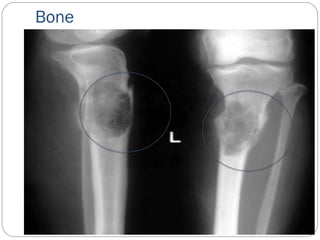
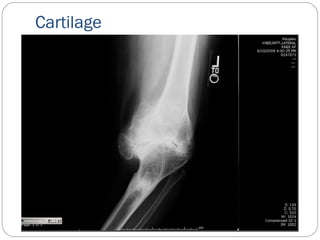
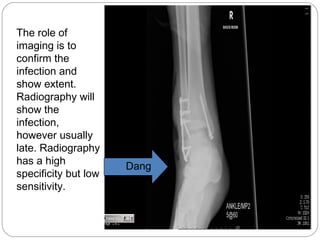
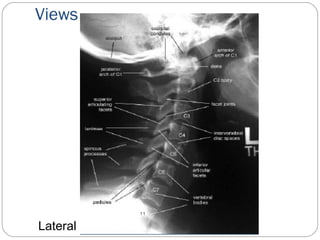
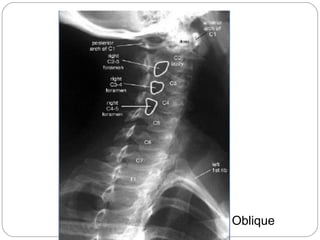
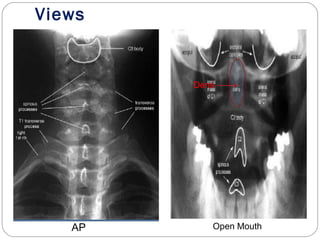
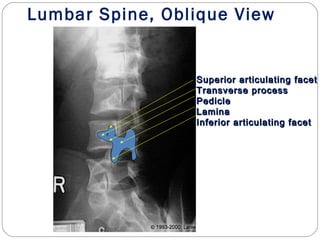
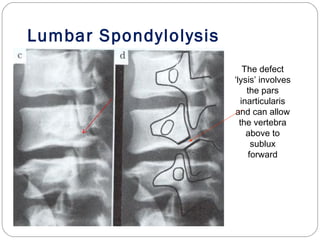
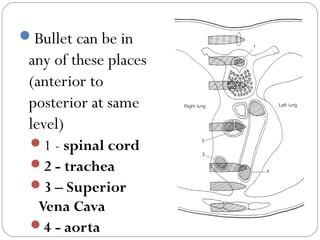
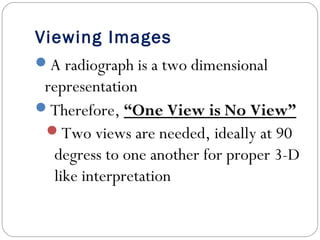
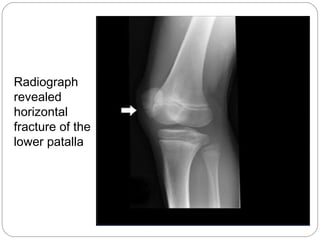
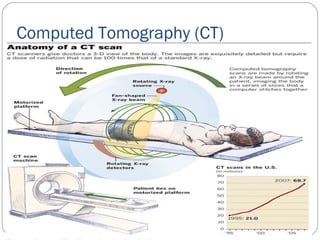
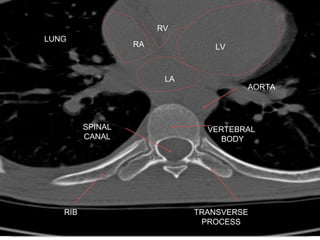
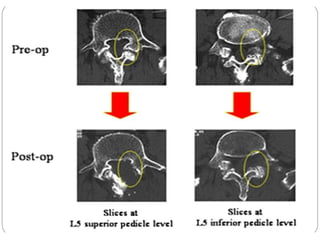
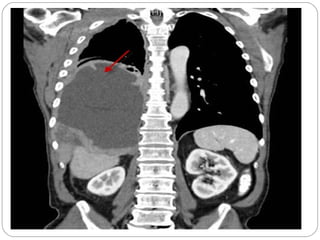
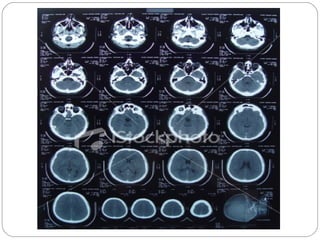
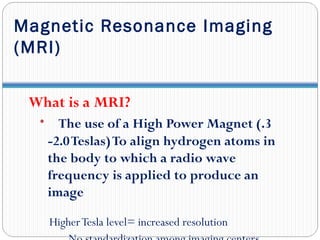
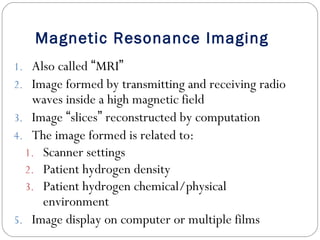
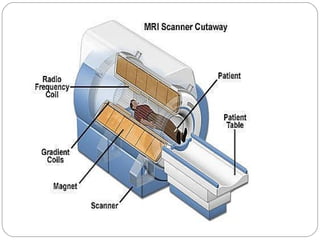
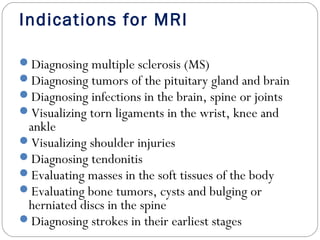
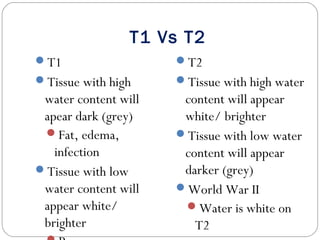
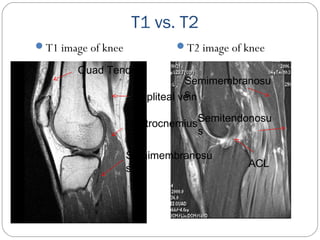
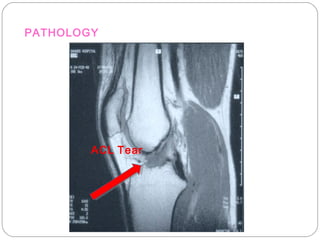
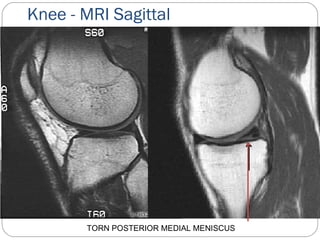
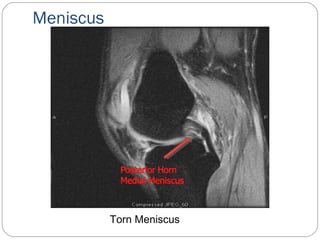
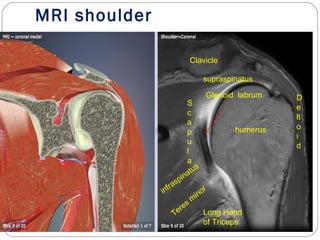
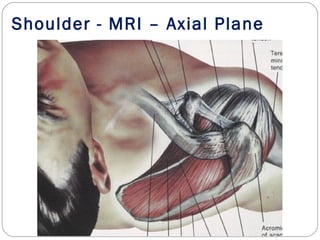
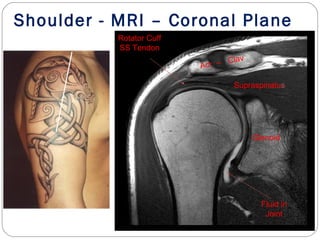
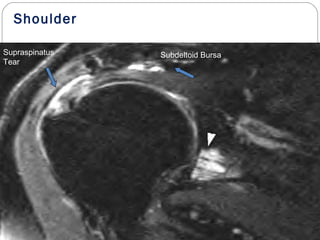
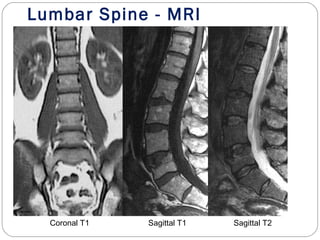
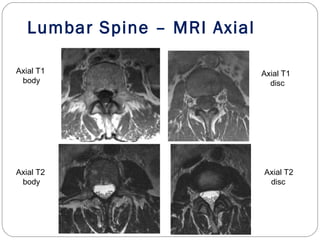
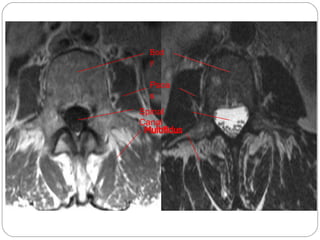
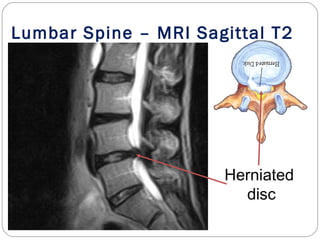
- Radiography provides static bone images but has limitations. CT and MRI produce cross-sectional "slices" and are better for soft tissue. CT uses ionizing radiation while MRI uses magnetic fields.
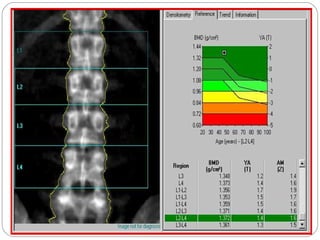
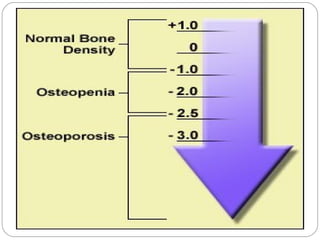
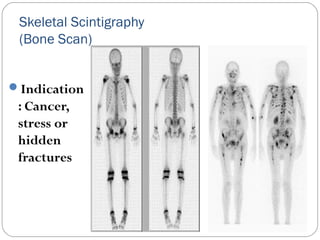
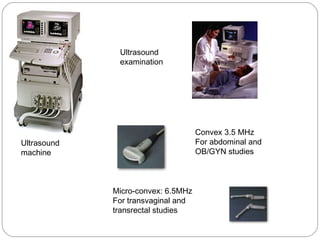
- Ultrasound uses soundwaves to image soft tissues. Nuclear imaging involves radioactive tracers to assess bone or joint function and disease activity. Each modality has advantages and limitations for different clinical purposes. Physical therapists should be familiar with common indications to select the appropriate imaging study.