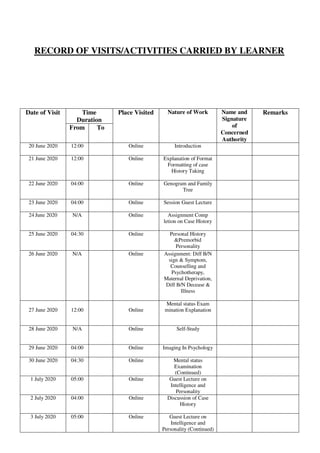
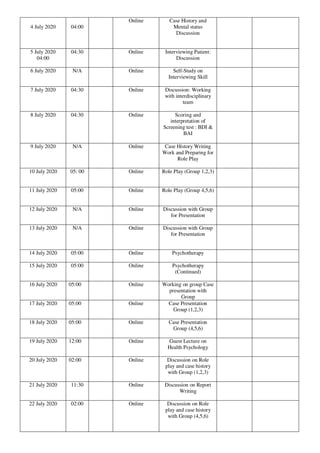
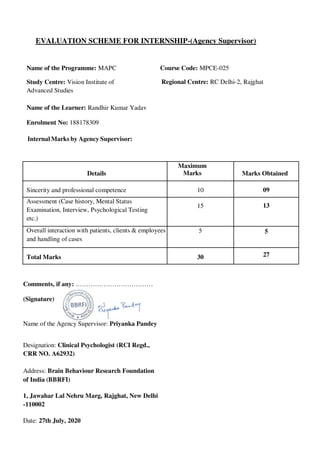
Randhir Kumar Yadav, an M.A. Psychology student at IGNOU, completed a 240-hour internship at the Brain Behaviour Research Foundation of India from June to July 2020, under the supervision of clinical psychologist Priyanka Pandey. The document includes a declaration of intent to intern, a reference letter requesting permission, records of online activities, evaluations by supervisors, and a certificate of completion. The internship provided an opportunity for practical experience in clinical psychology, complemented by guidance from experienced professionals.


















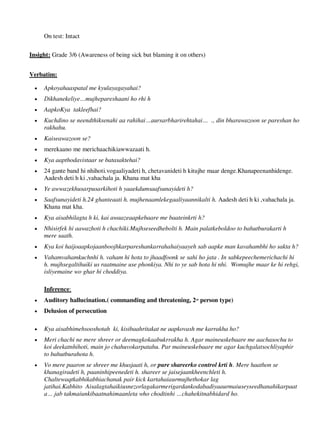































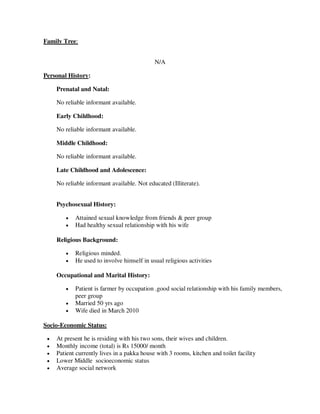
![FAMILY HISTORY:
• Nuclear family
• Family size- Normal [7 members], currently only 5 are living together
• Birth order- 3rd [1 elder brother and 1 elder sister]
• Interpersonal relations are good, major arguments happen occasionally, cordial
relationship between brother, sister and mother
• Supportive home atmosphere
• Father‘s birth mother died at the age of 25 years due to choking, grandfather got
remarried to current grandmother
• Grandfather did not disclose that the client‘s paternal father‘s mother was not biological
and hence father held a grudge against them. He was abusive towards his children.
• Mother had suicidal thoughts when pregnant with the client, wanted to take the children
and go elsewhere
• Client is close to elder sister
• Belong to upper middle class family, above average monthly income
• They follow Hindu religion but do not strictly believe in rigid ritualistic practices and
beliefs
• Father and brother consume alcohol occasionally
• Alcohol consumption by females is culturally acceptable in the family
• No social restrictions on females
PERSONAL HISTORY
Prenatal and Natal
• Pregnancy was full 9 months
• Type of birth: C-Section
• Mother faced complications while delivery
• Doctor said either mother or only child could be saved, but both of them were fine
• Normal cry at birth
• Client was born in a private hospital
Early Childhood
• Client was breast fed after delivery and continued for a small period of time
• Became lactose intolerant at 2 months
• Was bottle fed from thereon
• No eating problems
• Client started walking a little early, at the age of 7 months
• Started talking at a normal age
• Client started sucking both her thumbs at the age of 2 months and continued till father
scolded her at the age of 2 years
lOMoARcPSD|25238877](https://image.slidesharecdn.com/mapcmpce025internshipreportrky-241121163019-2044a657/85/IGNOU-Sample-Internship-File-for-MPCE025-64-320.jpg)