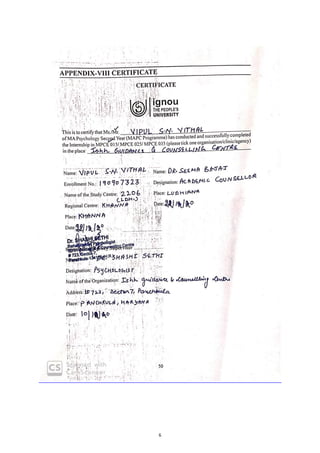
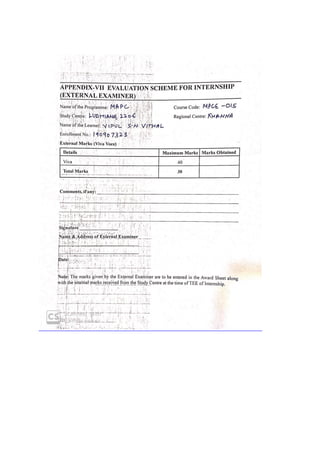
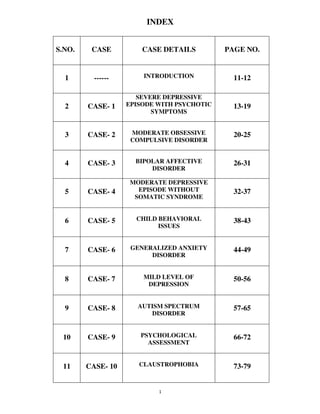
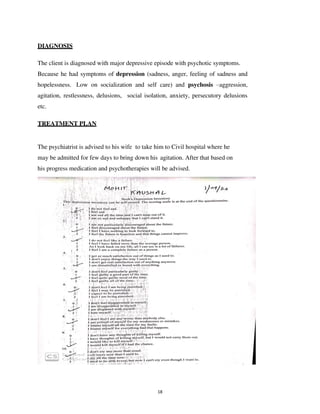
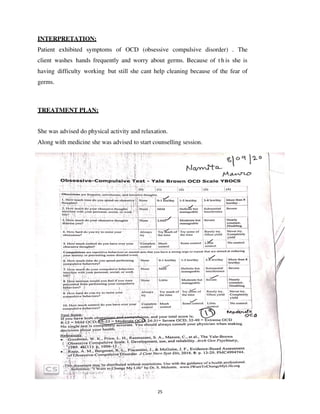
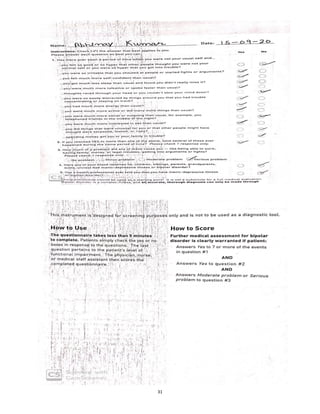
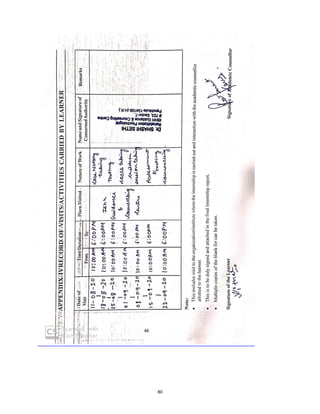
This internship report, submitted by Vipul S.N. Vithal to Indira Gandhi National Open University, presents an overview of his experiences and learnings in psychology through various case studies of mental health conditions. It emphasizes the importance of internships for practical exposure, professional development, and skill enhancement in the field of psychology, detailing objectives, case studies, and treatment plans. The report includes cases ranging from severe depressive episodes to obsessive-compulsive disorder, highlighting diagnostic processes and therapeutic approaches.